Information for patients
This leaflet can be made available in other formats including large print, CD and Braille and in languages other than English, upon request.
Introduction
This booklet has been created to help you gain a better understanding of your stay in the Critical Care Unit and to help you along your journey from Critical Care, to the ward and then to home.
It will allow you to understand why you feel a certain way and give you some reassurance and practical advice, as well as tips on how to deal with how you feel.
If you wish to discuss any part of this booklet or have questions that the booklet does not answer, please speak to a member of the Critical Care team as they will all be happy to help you.
What is the Critical Care Unit?
The Critical Care Unit, also known as the Intensive Care Unit (ITU), delivers specialised care for people whose conditions may be life threatening.
The level of care required is greater than on a ward and you will have required close monitoring and specialist treatments. That is why there are so many staff on the unit and it is usually one nurse to one or two patients, depending on the level of care required.
The staff working on Critical Care are highly trained in caring and treating people, like yourself, who require this level of care. The team consists of:
- Critical Care Consultant
- Critical Care Doctors
- Critical Care Nurses
- Critical Care Health Care Assistants (HCAs)
- Advanced Critical Care Practitioners (ACCPs)
- Physiotherapists
- Physiotherapy Assistants
- Occupational Therapist
- Dietician
- Pharmacist
- Speech and Language Therapist (SALT) – on request
- Housekeeper and Domestic Staff
The team are here to help support and actively rehabilitate you throughout your journey from Critical Care, to the ward, then into the community. As a team, we will be present to offer you and your family any assistance that is required with your rehabilitation.
Common Problems During & After a Critical Illness
All people can be affected differently due to the impact of critical illness.
All of the following symptoms can be normal following a hospital stay in Critical Care – it does not mean that these effects will last forever.
Effects of critical illness:
- Breathlessness
- Poor appetite
- Poor memory/concentration
- Difficulty problem solving
- Bladder and bowel dysfunction
- Hair loss/thinning
- Difficulty sleeping/staying asleep
- Strange memories/hallucinations
- Feeling anxious/low mood
- Fatique
- Skin sores/wounds
- Swallowing difficulties
- Increased sputum
- Communication difficulties including voice changes
- Decrease mobility
- Weakness
Rehabilitation
Rehabilitation helps you to be as independent as possible in your everyday activities; including work or hobbies. The rehabilitation will be personal to you, working towards shared goals.
The Physiotherapists (Physios) on Critical Care take the lead with rehabilitation and work with you to try to overcome the effects of critical illness by carrying out rehabilitation and exercise programmes. The programmes will be made up of tasks and goals aiming to improve functional strength and abilities.
Completing your rehabilitation will potentially reduce your length of stay in Critical Care and hospital and may reduce the chance of you being readmitted to hospital.
When you are ready to be discharged from Critical Care, the Physiotherapy Team will hand over to the Ward Therapy Team to let them know what you have been doing and outline a plan of how to progress.
The Ward Therapy Team will continue your rehabilitation input to progress you as much as possible, to get you ready for the community.
Patient Diaries
You may not remember everything that has happened to you during your time in Critical Care, especially if you were sedated or confused during this time.
Even with clear memories, the experience can be overwhelming and difficult to make sense of.
A diary may have been started whilst you were on Critical Care.
This diary will include accounts from members of staff who were involved in your care during your hospital stay. This can help you connect to what might feel like ‘somebody else’s story’.
Reading personal accounts of your care, words of support from staff, or even your own thoughts or feelings recorded on your behalf has been shown to help your recovery.
Before receiving your diary, a member of the Critical Care Team will offer to go through it with you. You might prefer to take it home to read later or you may wish not to read it at all.
During your Critical Care stay, photographs may have been taken of you and these photographs will be kept separate to the main part of your diary. We will always make you aware of any photographs.
Sometimes, people can find this distressing to see, as you may not realise how unwell you have been, but research shows this is commonly helpful in a patient’s recovery. If you do not wish to view them straight away, they will be kept for 6 months before being erased.
Critical Care Equipment
Waking up on Critical Care can be a frightening experience.
There are many machines, wires and alarms sounding around you and a lot of different health care professionals will visit to carry out assessments.
This can be quite scary and overwhelming.
To help you understand your surroundings the pictures shown in this booklet are of examples of some of the machines and attachments that you may have required. Not all patients require all of these.
Ventilator

A breathing machine, known as a ventilator helps patients with breathing problems. A breathing tube may be inserted into the trachea (windpipe) through the mouth, nose or sometimes via the trachea itself. As patient’s health and breathing improve, they can be weaned from the ventilator. This is known as intubation and ventilation
Monitor

A monitor is at each bedside recording vital signs such as heart rate, blood pressure and oxygen levels in the blood.
In order for this to work, you will have been connected to a number of leads. The monitor bleeps if the numbers change from the ‘’normal’’. The alarms draw the attention of the staff near you to check you are okay. You may remember hearing these alarms
Intravenous Infusion Pumps

Infusion Pumps are used to give medications and fluids through drips into the veins, sometimes through a line in the neck or groin called a central line.
These pumps may make different beeping sounds to alert staff.
CVVHD

A type of kidney filtration machine known as Continuous veno-venous haemodialysis (CVVHD) is used on ITU. This machine can be used to help take over the role of the kidneys and correct problems related to poor kidney function.
You may have been attached to this machine by a line in your neck or your groin.
MOTOMED

The MOTO med is an exercise bike, used in the bed, to help the movement and/or strength of your arms or legs.
You may have felt it move your limbs for you (passive movement) or you may have pushed it yourself (active movement) depending on level of consciousness.
Combilizer

The Sara Combilizer is a device that allows you to be repositioned into standing, laying and sitting positions when you are unable to do this yourself or need some help with doing this.
Tracheostomies and Endotracheal Tubes
During your stay on Critical Care you may have been placed on a ventilator. Whilst on the ventilator you will have had an endotracheal tube (ETT) inserted into your mouth or nose to assist with your breathing.
ETTs are long and flexible and have an inflatable balloon at the end of the tube known as a cuff. The cuff is inflated to keep the tube in your windpipe. The ETT is connected to the ventilator to help with your breathing.
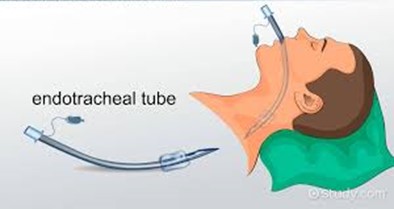
To wean you off a ventilator, the medical team may insert a tracheostomy. A tracheostomy is a tube which is inserted through a hole made in the neck. It allows you to be awake and comfortable whilst on a ventilator.
Most patients have the tracheostomy removed on Critical Care before being transferred to the ward. Tracheostomies are usually painless to remove and the opening in your neck does not require stitching as it will close naturally over time, leaving a thin horizontal scar.
Initially a tight dressing may have been placed over the tracheostomy site which prevents air going in and out and makes talking easier. Your voice may be weak or husky. Often this will improve spontaneously.
More information about tracheostomies can be found at:
https://icusteps.org/assets/files/information-sheets/tracheostomy.pdf

https://icusteps.org/assets/files/information-sheets/tracheostomy.pdf
Transfer to the Ward
When you no longer need Critical Care treatment you will be transferred to another ward. This is a positive step, but it can be difficult to adjust to the change.
While ward transfer is a sign of improvement and a step closer to going home, you and your family must adjust to less monitoring and having fewer staff close at hand. It is normal to feel apprehensive about this.
A member of the Critical Care outreach service will monitor you to ensure that your transition to the ward goes smoothly and that you continue to recover well for the days following discharge from Critical Care.
Different therapy teams will continue to see you on the ward to help progress your rehabilitation goals and help guide you with any exercises they have given you (including breathing exercises).
It is important to keep doing your exercises to help build your muscle strength.
Discharge Home
The decision for you to be discharged home from hospital will be made by your medical or surgical Consultant once your condition has improved.
Often additional discussion with the wider teams is needed to determine whether you are fit enough to manage safely at home on your own (with or without support).
The support that you require will vary depending on many factors including your personal circumstances, illness and length of hospital stay. Some patients require an additional period of time at a rehabilitation centre before returning home.
When you are ready to be discharged from hospital, your exercise plan and ongoing rehabilitation goals will be reviewed.
Your Physiotherapist and/or occupational therapist will decide whether you need further therapy once home. They will assess for any assistive equipment which you might need at home.
The therapists, nursing staff and discharge team can help identify and arrange any care support with day-to-day tasks that may be needed. This can include things like meal prep and washing/dressing help.
Getting back to everyday life
Once you have been discharged from hospital your recovery will be well underway, however many patients still have a long way to go before they begin to feel like themselves again.
While it is often an enormous relief to be home, you may find the first few weeks difficult in terms of readjusting to everyday life, and being without constant clinical care and support.
Getting back to work can be an additional worry for many Critical Care stayers. You may need a prolonged period of time recovering at home before you are able to think about returning to work. Your GP will be able to guide you here.
The following link can provide you with helpful information on when to return to work with helpful tips and advice on getting help from your employer.
https://gstt.criticalcarerecovery.com/file/returning-to-work-after-critical-care.pdf
Depending on the reason you were admitted to Critical Care, there may be no reason why you cannot get back to driving.
There may be reasons for caution around getting back behind the wheel, but if you are in any doubt about your ability to drive, please consult your GP and insurance company.
Rehabilitation and Recovery Tips
1. Breathlessness and Sputum
After an admission to Critical Care, many people often feel short of breath. Every day activities such as getting dressed, walking or everyday tasks can make you feel breathless. This can cause some people fear and panic.
These are some simple tips you can use to help improve how you are feeling:
- Square breathing: Breathe in slowly for 3 seconds, hold your breath for 3 seconds, breathe out through pursed lips for 3 seconds and rest for 3 seconds. This can be repeated 5 to 6 times in a row and you can increase or decrease the time as you need, do not force your lungs to empty.
- Breathing control during effort: Breathe in before you make the effort, breathe out whilst making the effort i.e. lifting, sitting to standing.
- Positions:
1) Side lying with your upper arm propped onto a pillow and a pillow between your legs helps support the muscles involved in breathing.

2) Tripod position, experiment with your arm position to find what is comfortable for you. You can also use pillows to prop your arms up.


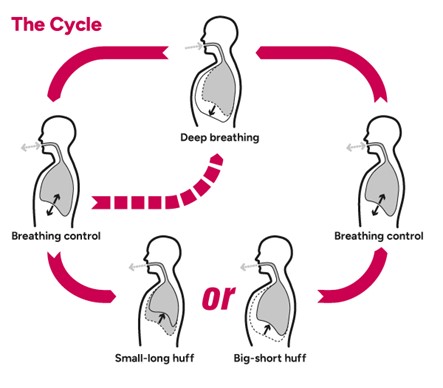
- Secretion management: You may find that you have trouble clearing secretions (phlegm) from your chest and this may cause you to feel breathless. The active cycle of breathing technique (ACBT) can help you breathe easier, loosen and clear phlegm and improve your cough.
Breathing Control: Breathe in and out gently through your nose or mouth (If mouth breathing use ‘pursed lips breathing.
Deep Breathing Exercises: Take a long, slow, deep breath in, through your nose if you can., Breathe out gently and relaxed, like a sigh. You should do 3 to 5 deep breaths. Some people find it helpful to hold their breath for about 2 to 3 seconds at the end of the breath in, before breathing out.
Huffing: A huff is exhaling through an open mouth and throat which helps move sputum up your airways. To ‘huff’ you squeeze air quickly from your lungs, out through your open mouth and throat, as if you were to mist up a mirror or your glasses.
There are 2 types of huffs:
The small-long huff (for low down phlegm): Take a small to medium breath in and then huff the air out until your lungs feel quite empty.
The big-short huff (for high up phlegm): Take a deep breath in and then huff the air out quickly. This should clear sputum without coughing.
For Information
Available:
https://www.acprc.org.uk/media/521payl5/gl-05acbt-1.pdf
2. Fatigue Management
Fatigue can be both physical and mental and often described as overwhelming.
It could feel like having no energy, being more tired than usual, more emotional than normal or having problems sleeping. This usually lasts a few weeks but it may last longer.
Below are some simple tips you can use to help manage fatigue:
- Spreading your activities out over the course of the day.
- Prioritising what needs to be done and what can wait a little longer.
- Taking frequent breaks.
- Trying to be organised to avoid unnecessary trips.
- Concentrating on one activity at a time.
- Sitting rather than standing when completing tasks.
- If you normally use inhalers for a lung problem, have these with you.
- Ask others for help.
3. Mobility and Physical Activity
It is very common and expected for your body to feel weaker and to have reduced movement in your joints and reduced muscle mass. When you are walking, you might feel unbalanced and may not be able to walk as far, or as you have previously been able to do.
This is all normal after a critical illness but it is important to complete exercises to regain this strength and movement. Below are some examples of exercises you can complete.
You should choose 4 to 5 exercises to start off and gradually build the number up as fatigue allows. You should aim to complete 5 to 10 repetitions of each exercise up to 4 times per day. Please speak to your Physiotherapist if you have any questions or concerns with the exercises as these should not be painful.
Note: Please see the useful resources and contacts at the end of the document for hyperlinks of the following exercises and more. These links include ways to make the exercises easier and harder.
Bed Exercises
Ankle Dorsiflexion + Planar Flexion

Start by lying on your back in bed, point your feet towards your face and then point them away from your body. Your knees should always remain straight throughout exercise.
Static Quads

Lie on your back in bed, with both legs straight and relaxed. Tense your thigh muscles and push your knee down into the bed, one leg at a time, and hold for approximately 5 seconds as able.
Straight Leg Raise
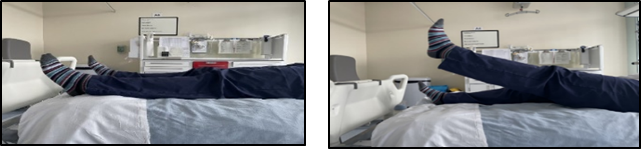
Lie on your back in bed, with your legs straight. Raise your left leg off the bed as high as possible and hold for approx. 5 seconds. Return to the starting position and repeat the exercise with your right leg.
Bridging

Lie on your back with your knees bent and your feet flat on the bed. Squeeze your stomach muscles in, then lift your bottom off the bed. Hold for about 5 seconds, then gently lower.
Hip Abduction + Adduction

Lying on your back in bed, start with your legs straight and together. Move one leg out to the side, then bring the leg back in again. When completing this exercise, keep your foot pointing up towards the ceiling throughout.
Frontal Raises

Lie on your back with your arms down beside your body. Lift one arm so that it is straight in the air, making sure you keep your elbow straight and hold for about 5 seconds. Gently lower it back to the bed beside your body. Make sure each repetition is slow and controlled.
Elbow Flexion

While in bed (sitting up or lying down), tuck your elbow into your ribs with arms down by your side. Bend your elbow, bringing your hand towards your shoulder and return to normal position. Make sure each repetition is slow and controlled.
Shoulder – Internal + Rotation

While in bed (sitting up or lying down), tuck your elbow into your ribs and place your elbow at a 90-degree angle. Rotate your arm away from the body approximately 45 to 90 degrees, depending on your normal shoulder movement, and return to normal position. Make sure each repetition is slow and controlled.
Chair Exercises
Heel Raises and Toe Taps

In sitting, place both feet flat on floor. Heel raises: Push your toes into the ground to raise your heels off the floor. Toe Taps: Push the heels of your feet into the ground, raising your toes off the ground.
Front and Lateral Raise

In sitting, place your arms down beside your body. Front: Lift one arm straight out in front of you. Lateral: Lift one arm out to the side. Make sure, you keep your elbow straight and hold for approximately 5 seconds. Gently lower it back down to the start position. Make sure each exercise is slow and controlled.
Elbow Flexion

While seated, place your elbows by your side at a 90-degree angle and make a fist with your hands. Fully straighten your elbows out in front of you and pull your fists back towards your chest in a rowing motion.
Knee Extensions

In sitting, place your feet flat on the floor with your knees at a 90-degree angle. Extend your leg out in front, so your leg becomes straight. Hold your leg out straight for approximately 3 seconds and control the movement back to the starting position.
Marching in Sitting

Sit upright with your feet placed flat on the floor and shoulder width apart. Bring your right knee up towards your chest and return to starting position. Repeat with your left knee.
Punching in Front

While seated, tuck your elbow into your sides with your arms’ resting on the armchair. Bring your arm straight out in front of your body. Make sure each repetition of the exercise is slow and controlled and return to the starting position.
Standing Exercises
Full Moons

Standing upright, place your hands by your side with your palms facing towards your thighs. Keep your elbows slightly bent and raise your arms out to the side. Once in a horizontal position, turn your arm so that the palms of your hands are facing forward and continue to raise your hands above your head.
Heel Raises

Stand with your feet shoulder width apart and raise both heels off the floor, with your toes firmly on the ground. Keep your knees straight throughout the exercise. If this is too hard hold onto a firm, counter or chair for support.
Mini Squat
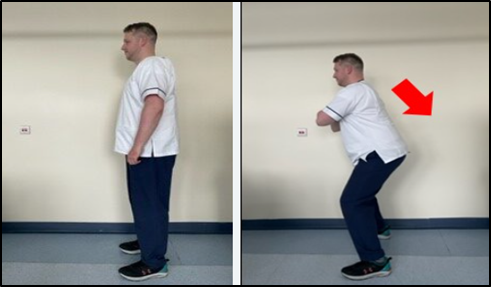
Stand with your feet shoulder width apart. Keep your head and chest upright, and spine in a neutral position. Slowly push your hips back and bend your knees.
Marching on the Spot

Standing shoulder width apart, bring one knee up towards your chest and place back onto the floor. Repeat with the other leg and alternate this.
Standing Kickbacks

Stand with your legs together, facing a supportive surface/wall. Place a hand on the surface/wall. Keeping your leg straight, raise one leg back away from your body then return to the starting position. Repeat this with the other leg and alternate.
Wall Press-ups

Stand facing a wall. Place both hands on the wall and position your hands shoulder width apart with your fingers pointing up to the ceiling. Bend your elbows and bring your chest towards the wall. Straighten your arms to return to the starting position and repeat the exercise.
4. Nutrition
As a response to severe illness the body uses up its own muscle and fat stores for energy. Losing weight and muscle wasting are very common symptoms associated with critical illness.
To have unplanned weight loss, or being a low weight for your height is not good for your recovery. It is important to manage your nutrition as this helps with reducing infection risk, strengthening your immune system, helping your body recover and get stronger and potentially reducing your length of stay in hospital.
Eating and drinking as normal after critical illness can be difficult for many reasons. If this is a problem, you may need to have support with this. This may include being fed through a tube into your stomach (nasogastric tube (NG)) or your bowel (nasojejunal (NJ)). You may need nutrition delivered into the blood stream (total parenteral nutrition (TPN)) or nutritional supplements.
You may also find your appetite is reduced and find eating difficult. This could be due to many reasons such as food tasting different, your mouth being dry, you feel too tired or weak to eat or you are experiencing symptoms that stop you wanting to eat such as diarrhoea, constipation or vomiting.
If you experience any of the above problems, here are some tips to help you with eating during your recovery.
- Eat ‘little and often’ such as small portions 6 times a day as this may be easier than eating larger meals.
- Eating products high in calories and protein alongside meals can help gain weight and provide energy.
- Eat slowly and try to relax whilst eating.
- Ensure you are in a good eating position.
- Heavy, fatty foods may be difficult to digest so choose these less often if you do find them difficult.
- Try to avoid filling up on drinks just before eating.
- Consider multivitamins if you struggle to reach your 5 fruit and vegetable a day.
- Aim to include a portion of meat, fish, beans, soya protein or cheese at each meal.
Please see the useful resources for documents containing more information.
5. Swallowing
If you face difficulties with eating, drinking and/or swallowing after critical illness, this can be due to a number of factors. These can include: altered taste, reduced appetite, breathlessness and fatigue, muscle weakness or the need to have been intubated.
You may have been seen by speech and language therapists in hospital who may have given you advice on self-management or exercises to complete.
These might include:
- Being sat upright when drinking/eating and taking smaller sips/bites.
- Not eating or drinking when you are tired or breathless.
- Choosing softer foods that do not require as much chewing.
If you notice any of the following symptoms, then contact your GP who can refer you on to the relevant teams:
- Coughing or choking when eating or drinking.
- A wet or gurgly voice after swallowing.
- A sticking sensation in the throat when eating or drinking.
- Frequent chest infections.
6. Psychological impacts and recovery
Sleep and Delirium
During your Critical Care stay your sleeping pattern may become irregular, it may be more difficult to fall asleep or your usual sleep pattern may be broken. Once you step down to the ward and become more active your sleeping should improve as you will use more energy throughout the day.
If you have been sedated for a number of days in Critical Care, you may find your body clock is disrupted. If you feel very tired, then a nap may be helpful, but try not to sleep too long during the day. This is because it is important to get your day and night routines back to normal.
Some people may suffer from nightmares following a Critical Care stay. These can be very vivid and frightening at times. These usually reduce, and stop, over a few days or weeks.
Some patients also experience delirium whilst in hospital. This is usually where people see or hear things which are not there, known as hallucinations. These thoughts or memories seem real but are not. They are caused by the combination of being critically ill and the medications that are given to keep you comfortable.
Delirium is usually temporary and resolves as the illness improves, but it can make people become agitated or aggressive (hyperactive delirium) due to the frightening things they are experiencing. Also people may appear very still and quiet due to internal thoughts (hypoactive delirium).
It is important to try to speak to close friends or family about your thoughts and feelings. They may also be able to help explain some of the things you are feeling and may not remember from your time being unwell.
If you are suffering with any new confusion at home, then please seek medical attention.
Anxiety and Depression
When we have feelings associated with worry, stress, or feel in danger, our body produces adrenaline. Adrenaline is a chemical that helps us take action on the ‘problem/feeling’, so we can deal with or escape from the situation (fight or flight) and this can cause the feeling of anxiety.
Once the problem has been solved, the adrenaline leaves the body and we return to a state of calm. This is nature’s way of helping us to cope with negative situations.
When problems cannot be overcome, the body will continue to produce adrenaline and feelings of anxiety. Feelings of increased anxiety may occur following a Critical Care stay due to frightening events, memories or thoughts you may have experienced, as can worries about the future following your Critical Care stay.
Learning about ways to manage your worry or anxiety can help; this is discussed in the self-care section, which is later in the leaflet.
Any worrying thoughts or memories of Critical Care should naturally fade over time but please contact your GP or speak to a member of staff on Critical Care if you are concerned.
Signs and symptoms of anxiety can be:
- Feeling restless,
- Uncontrolled worrying,
- Increased heart rate or breathing rate,
- Trouble concentrating,
- Irritability,
- Muscle tension,
- Disturbed sleep pattern.
Low mood is also common after being critically ill and feelings can range from sadness to despair. This is normal as your mind processes what you have been through and you make the transition from being dependant, back to independent. Try to keep active, as inactivity can lead to a lack of motivation and feelings of helplessness.
Signs of depression include:
- Sadness,
- Tearfulness,
- Poor appetite,
- Early waking,
- Loss of interest in things that were once enjoyable to you,
- Loss of interest in appearance.
Self-Care
Sometimes when we are dealing with difficult thoughts and feelings it can be easy to get lost in them. This is a common experience for many and can be unsettling if unexpected. Below are a few tips you can use to help manage your thoughts and feelings.
Mindfulness and grounding exercises:
These exercises can help reduce anxiety by teaching you how to focus on the moment we are in at present and not to think of the past or the future.
1. Breathing exercises (discussed in the breathlessness section) can be very helpful such as:
- Square breathing – visualise a square, follow each side breathing in a count of 3, hold for 3, out for 3, hold for 3 and back to the start.
- Pursed Lip breathing.
2. Grounding strategies:
It can be useful to have a ‘grounding technique’ to help you remind yourself and your body that you are safe. Below are three techniques you can use:
- Having a ‘grounding object’ – this is an object you focus all your senses on. For example: how does it feel, is it smooth, rough, light or heavy? What colour is the object, what shape, etc. When you use your senses in this way, it helps ground you in the here and now and reminds your brain and body where you are and that you are safe.
- Being aware – pick a small spot in the room. It could be anywhere, i.e. the corner of a door or some wallpaper. Now describe 5 things you notice about that small area. Colours, shapes, textures, etc. You do not need to rush this, take your time. Once you have noticed five things, see if you can notice any more. If you need to continue grounding, you can pick another spot and continue the exercise.
- Creating a safe space – this can be a real place which you can go to or a place you imagine in your mind where you feel safe. It is important that this place is easily accessible if it is real. You can fill this place with things that bring you comfort, real or imaginary, for example a warm blanket, happy photos or a scented candle.
3. Staying connected:
During your recovery, it is important to stay connected with family and friends, to discuss any thoughts and memories you have. This can be face-to-face, via phone call, text or video call. Whilst in hospital, you can access a number of services to aid with staying connected, such as virtual visiting, free Wi-Fi and flexible visiting times, including John’s campaign. Please discuss this with the ward staff for more information.
4. Reconnecting with activities:
What did you used to enjoy at home or in your social life? Start to complete some manageable activities that give you a sense of relaxation, pleasure and achievement. Remember to be kind to yourself and set realistic goals.
Recovery and Hospital Follow-up
The consultant will decide when you are ready to be discharged from hospital after discussion with members of the multi-disciplinary team. These may include Physiotherapists, Nurses, Occupational Therapists, Dietetics, Speech, and Language Therapy.
The support you may require on hospital discharge will depend on your own personal circumstances. Your rehabilitation does not finish when you leave hospital. The teams involved in your care will advise you on the most appropriate level of care to suit your needs.
You may have been advised to complete home exercises or referred into a community team, for continued therapy at home. Sometimes it is advised that you go to a rehabilitation centre, for ongoing Physiotherapy.
If the Multi-Disciplinary team all agree that going home will be a safe environment to which you can return, they will support you and your family to achieve this. You may be seen by Occupational Therapy who may assess your needs and provide you with equipment.
It may also be appropriate for you to go home with a new package of care or a change in the care you were usually provided.
At approximately 3 months after your hospital discharge, you may be invited to attend an outpatient follow-up appointment at the hospital. This is carried out by staff members from Critical Care including a Consultant, Nurse and Physiotherapist.
During this appointment we will discuss your progress and rehabilitation since hospital discharge and also if there is any further support you require. You will also have the opportunity to visit the Critical Care Unit if you wish to see those who were involved in your hospital stay.
Useful Contacts
Contact details for North Tees Hospital:
Hospital Switchboard
Telephone: 01642 617 617
Critical Care Unit
Telephone: 01642 382 720 or 01642 382 820
Chaplaincy Team
Telephone: 01642 383 138 For non-urgent enquiries, leave a message on the answer phone
website: https://www.nth.nhs.uk/resources/chaplaincy-team/
Please note: The Trust has a team of Chaplains who are there to offer impartial, non-judgemental and accessible care to everyone – patients, visitors and staff – that would benefit from someone to talk to.
This support is open to everyone. You do not have to follow a particular faith to speak to the chaplains. Chaplains simply facilitate pastoral, spiritual and, if appropriate, religious care at any point of your care.
Further Information
North Tees and Hartlepool NHS Foundation Trust. Links to exercise booklets:
- Standing Exercises
website: https://www.nth.nhs.uk/resources/standing-exercises/
- Chair Exercises
website: https://www.nth.nhs.uk/resources/chair-exercises/
- Bed Exercises
website: https://www.nth.nhs.uk/resources/bed-exercise/
- Asthma UK
A keep active advice handbook for people living with a lung conditions.
website: https://www.asthmaandlung.org.uk/living-with
- ACPRC
The Active Cycle of Breathing Techniques how to guide. Available:
website: https://www.acprc.org.uk/Data/Publication_Downloads/GL-05ACBT.pdf
- ICU Steps
This is a website founded by ex ICU patients, relatives and staff to support patients. There are many useful resources on this website:
website: www.icusteps.org
- ICU Steps Extra
Information around Nutrition in hospital after critical illness.
website: https://icusteps.org/assets/files/information-sheets/nutrition-in-hospital.pdf
- ICU Steps Extra
Nutrition at home after critical illness.
website: https://icusteps.org/assets/files/information-sheets/nutrition-at-home.pdf
- Intensive Care Society (ICS)
Aiming to further education and research into intensive care in the UK. The Intensive Care Society is the largest multi-professional intensive care membership organisation in the United Kingdom.
website: www.ics.ac.uk
- Headway
Promotes understanding of all aspects of brain injury. Providing information, support and services to people with brain injuries, their families and carers.
Helpline: 0808 800 2244
webisite: www.headway.org.uk
- ICNARC
Dedicated to improving intensive care treatment and helping patients get better sooner, with fewer complications.
website: https://www.icnarc.org/
- Cruse Bereavement Care
Provides counselling, support, information, advice, education and training services to friends and relatives of someone who has passed away, to help them understand their grief and cope with their loss.
Helpline: 0844 477 9400, Young Person’s helpline: 0808 808 1677
website: https://www.ataloss.org/FAQs/cruse-bereavement-care-tees-valley
- Citizens Advice Service
Helps people deal with their legal, money, housing and other problems by providing free, independent and confidential advice.
website: www.citizensadvice.org.uk
- Carers UK
Offers support and a sharing experience for carers.
website: http://www.carersuk.org
Acknowledgement
Some work in this booklet, is quoted and adapted with kind permission from:
ICU Steps
Road to Recovery: Critical Care rehabilitation guide
Comments, concerns, compliments or complaints
Patient Experience Team (PET)
We are continually trying to improve the services we provide. We want to know what we’re doing well or if there’s anything which we can improve, that’s why the Patient Experience Team (PET) is here to help. Our Team is here to try to resolve your concerns. The office is based at the University Hospital of North Tees if you wish to discuss concerns in person. Our contact details are:
Telephone: 01642 624719
Freephone: 0800 092 0084
Opening hours: Monday to Friday, 9:30 a.m. to 4:00 p.m.
Email: [email protected]
Out of hours
Out of hours if you wish to speak to a senior member of Trust staff, please contact the hospital switchboard who will bleep the appropriate person.
Telephone: 01642 617617
Patient, Public and People with Lived Experience
We are looking for patients to share their experiences of healthcare and to join our Involvement Bank. Working with the patients, carers, families and the general population we support in making decisions about their care can lead to better health outcomes, increased patient satisfaction and a better overall experience. We want to listen and work with you in shaping the future of your healthcare services. To find out more about the Involvement Bank go to our website or contact us at:
Website: www.nth.nhs.uk/about/community/people-with-lived-experience
Email: [email protected]
Data protection and use of patient information
The Trust has developed Data Protection policies in accordance with Data Protection Legislation (UK General Data Protection Regulations and Data Protection Act 2018) and the Freedom of Information Act 2000. All of our staff respect these policies and confidentiality is adhered to at all times. If you require further information on how we process your information please see our Privacy Notices.
Telephone: 01642 383551
Email: [email protected]
Privacy NoticesLeaflet feedback
This leaflet has been produced in partnership with patients and carers. All patient leaflets are regularly reviewed, and any suggestions you have as to how it may be improved are extremely valuable. Please write to the Clinical Governance team at:
Email: [email protected]
Leaflet reference: PIL1555 – Version 01
Date for Review: 12th February 2028