Information for patients
This leaflet can be made available in other formats including large print, CD and Braille and in languages other than English, upon request.
Your doctor has advised you to have a Transoesophageal Echocardiogram (TOE) to take detailed images (pictures) of your heart. This leaflet will help you understand what will happen before, during and after the procedure.
How does my heart work?
Your heart is a muscle that pumps blood around your body. Sometimes people are born with or develop problems with the heart’s muscle, the chambers (ventricles and atria) or the structures within the heart such as the valves.
What is a TOE?
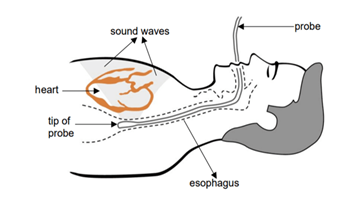
This test allows us to scan the heart’s structure and function using ultrasound (a painless examination using sound waves) to take detailed pictures. Ultrasound is safe and no radiation (X-rays) is used.
It is like a standard echocardiogram (echo) but a TOE involves placing a small flexible tube into your oesophagus (the tube your food goes down) and stomach.
This gives your doctor clearer and more accurate pictures than a standard echo, as the oesophagus lies just behind the heart and there is no interference (unwanted signals) from the ribs or lungs.
You will be offered a local anaesthetic spray to the back of your throat and light sedation at the start of the procedure. The sedation will make you feel relaxed but not asleep.
What are the risks and possible complications?
TOE is a safe procedure but does have some risks and possible complications. These will be discussed fully before you consent to the procedure. The risks must be compared to the benefits and your doctor will have considered these.
The risks and possible complications include:
- Aspiration. If you are sedated and your stomach contains food and drink it can leak into your lungs, affect your breathing and cause an infection. This is one of the reasons why you must not eat or drink for 6 hours before the procedure.
- Perforation (hole) or a tear of the wall of the oesophagus. This can happen to 1 to 3 patients in every 10,000. This is unlikely unless you have had a previous history of problems with your oesophagus.
- Pleeding. If any bleeding occurs, steps will be taken to stop it.
- Sore throat. You may have a sore throat for 24 to 48 hours.
- Damage to teeth or bridge-work. The probe can occasionally cause damage to teeth or bridge-work. This is rare as a mouth-guard is used to minimise (reduce) the risk.
- Conscious light sedation. This can sometimes cause problems with breathing, heart rate and blood pressure.
- Discomfort. You may feel some discomfort during the procedure, we try to keep this to a minimum. A nurse will be with you throughout the procedure and if you show signs of being uncomfortable, steps will be taken to relieve this.
You must tell your doctor if you have had treatment such as surgery to your oesophagus, or if you know you have a narrowing of your oesophagus as these could increase the risks during the procedure.
What will I need to do to prepare for my procedure?
You should not eat or drink for 6 hours before your appointment.
It is important to arrange for someone to take you home and, if you have had sedation, stay with you for 24 hours after the procedure. You must not drive, operate machinery, be in charge of young children or drink alcohol for 24 hours after the procedure.
Depending on the type of job you do you may need to arrange time off work. Your doctor or nurse can discuss this with you.
You can expect to be at the Unit for about 3 hours. There is limited space so only in special cases will anyone be allowed to stay with you, for example, patients with special needs.
Unless advised you should use your inhalers and take your tablets or medicines as usual. You may take these with a small amount of water.
There is no need to stop taking blood thinning tablets such as Warfarin, Apixaban, or others including Clopidogrel or Aspirin before the procedure. Please bring a list of all your medication (drugs) with you to your appointment.
You will be given a hospital gown to wear during the procedure and may wish to bring a dressing gown and something to read while you wait. Please bring your reading glasses (if you use them) as you will need to read and sign a consent form.
Please do not bring any valuables, jewellery or large amounts of money as we are unable to accept responsibility for any loss or damage.
Where will I go to have my TOE?
Your procedure will usually be performed at the Cardiology Day Unit at the University Hospital of North Tees.
You will be sent a letter telling you when and where to come.
It is important you arrive at your appointment time so we can prepare you for your procedure and answer any further questions you may have.
Who will be present during my procedure?
A team of healthcare professionals, including a cardiologist (a doctor who specialises in the heart), nurses and an echocardiographer (someone who is trained to carry out echoes).
North Tees and Hartlepool NHS Foundation Trust is a teaching organisation. We could not train future doctors, nurses or other health professionals without the co-operation of patients. You will be informed if there are to be any observers present.
Healthcare professionals in training may take part in your procedure according to their experience and stage of training. They will be supervised by fully qualified staff at all times.
What will happen when I arrive for my procedure?
You will be shown to a bed in a screened area. Your doctor or nurse will explain the procedure again and ask you to sign a consent form.
You will need to undress and put on a hospital gown, but can keep underwear on your bottom half.
Your blood pressure, pulse and temperature will be checked. A cannula (a fine tube) will be inserted into a vein in your arm or the back of your hand using a small needle. This allows medication such as sedation to be given.
You will be asked to remove any glasses, contact lenses or loose fitting dentures just before the procedure.
What will happen during the procedure?
The whole procedure takes up to 90 minutes but the time that the probe is in the body is about 15 to 20 minutes. You will be taken to the procedure room on your bed. You will be connected to equipment to monitor (check) your heart rate and rhythm, blood pressure and blood oxygen levels.
Your throat will be sprayed with local anaesthetic to numb the area and a plastic mouth guard placed between your teeth. You will be asked to lie on your left side. Sedation may be given, if needed. A nurse will stay with you to make sure you are comfortable.
You will be asked to swallow as the probe is inserted and passed into your oesophagus (gullet).
Your doctor and echocardiographer will record a series of moving pictures of your heart.
When the procedure is finished the probe is removed.
What happens after the procedure?
After the procedure you will be taken back to your bed in the unit to rest and a nurse will continue to monitor your blood pressure, pulse and temperature regularly. The cannula will be removed from your hand or arm.
Before you go home, your doctor will see you again with the results of the scan. They will discuss with you the findings and further tests or treatment choices that might be needed. They will answer any questions you may have.
You are encouraged to ask a family member or friend to be present for this discussion in case the sedation makes it difficult for you to remember details of what has been said to you about the test result and plan.
If you have had sedation you may feel sleepy and will need to stay for 1 to 2 hours after the procedure.
If you have not had sedation you may be able to get dressed and go home after about 30 minutes to 1 hour.
You should not eat or drink for 30 minutes and have nothing hot for 1½ hours until the spray to numb your throat has worn off.
If you have had sedation a responsible adult must take you home and stay with you for 24 hours.
How will I feel when I go home?
You may:
- feel tired for up to 12 hours.
- have a sore throat for up to 36 hours.
You should:
- relax quietly at home for the rest of the day.
- eat, drink and take any medications as normal unless your doctor has advised otherwise.
You must contact the Unit (see contact numbers at the end of the leaflet) where you had your TOE, immediately if you:
- have severe pain in your neck, chest or abdomen.
- develop a temperature higher than 38°C (100.4°F).
- develop vomiting (being sick) or nausea (feeling sick).
If the unit is closed and you have an urgent problem the night after your procedure you should contact NHS 111 or 999.
What activities should I avoid when I go home?
If you have had sedation the effect will stay with you for
24 hours so it is important you follow this advice.
Due to the effects of sedation, for the first 24 hours you:
- must not go back to work.
- must not make any important decisions or sign any legal documents.
- must not operate any machinery or electrical appliances.
- must not drive a car, ride a bicycle or motorcycle. It is an offence to drive while unfit to do so because of drugs used during your sedation and it will probably invalidate your insurance policy.
- must not supervise children.
- must not drink alcohol.
- must not take sleeping tablets or tranquillisers unless advised by your doctor.
- must not go near open flames or sources of high heat.
- must not lock your toilet or bathroom door in case you need any help.
- should not smoke.
Will I need a follow-up appointment?
The results of the test will be sent to your doctor. You may be sent an appointment through the post to come for a follow-up appointment with a cardiologist.
Your GP will also receive a copy of the results.
Contact numbers
University Hospital of North Tees
Cardiology Day Unit
Telephone: 01429 522020
Monday to Friday, 8.30am to 5.00pm
If no reply leave a message or telephone: 01429 522021
Non-urgent messages can be left at any time on the answering machine.
Further information is available from:
NHS Choices
Telephone: 111 (when it is less urgent than 999)
Calls to this number are free from landlines and mobile phones
or via the website at www.nhs.uk
British Heart Foundation
Telephone: 020 7554 0000
Heart Helpline: 0300 330 3311
Monday to Friday, 9.00am to 5.00pm
or via the website at www.bhf.org.uk
British Society of Echocardiography
Website at www.bsecho.org
British Heart Foundation Video of TOE procedure
The Cardiology Department of North Tees and Hartlepool NHS Foundation Trust run an active research programme of clinical trials. If you are interested, please ask your consultant or nurse if there are any suitable trials to participate in.
Comments, concerns, compliments or complaints
Patient Experience Team (PET)
We are continually trying to improve the services we provide. We want to know what we’re doing well or if there’s anything which we can improve, that’s why the Patient Experience Team (PET) is here to help. Our Team is here to try to resolve your concerns. The office is based at the University Hospital of North Tees if you wish to discuss concerns in person. Our contact details are:
Telephone: 01642 624719
Freephone: 0800 092 0084
Opening hours: Monday to Friday, 9:30am to 4:00pm
Email: [email protected]
Out of hours
Out of hours if you wish to speak to a senior member of Trust staff, please contact the hospital switchboard who will bleep the appropriate person.
Telephone: 01642 617617
Patient, Public and People with Lived Experience
We are looking for patients to share their experiences of healthcare and to join our Involvement Bank. Working with the patients, carers, families and the general population we support in making decisions about their care can lead to better health outcomes, increased patient satisfaction and a better overall experience. We want to listen and work with you in shaping the future of your healthcare services. To find out more about the Involvement Bank go to our website or contact us at:
Website: www.nth.nhs.uk/about/community/people-with-lived-experience
Email: [email protected]
Data protection and use of patient information
The Trust has developed Data Protection policies in accordance with Data Protection Legislation (UK General Data Protection Regulations and Data Protection Act 2018) and the Freedom of Information Act 2000. All of our staff respect these policies and confidentiality is adhered to at all times. If you require further information on how we process your information please see our Privacy Notices.
Telephone: 01642 383551
Email: [email protected]
Privacy NoticesLeaflet feedback
This leaflet has been produced in partnership with patients and carers. All patient leaflets are regularly reviewed, and any suggestions you have as to how it may be improved are extremely valuable. Please write to the Clinical Governance team at:
Email: [email protected]
Leaflet reference: PIL1096 version 2
Date for Review: October 2028