Information for patients
This leaflet can be made available in other formats including large print, CD and Braille and in languages other than English, upon request.
Introduction
This leaflet tells you how to treat a rectal prolapse.
What is a Delorme’s procedure?
It is a procedure to repair a rectal prolapse.
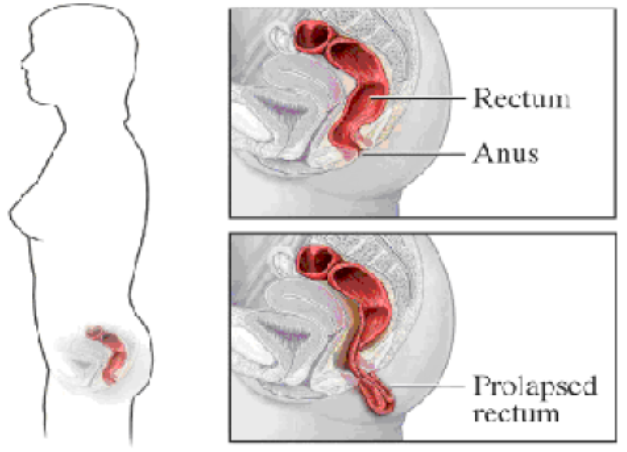
What is a rectal prolapse?
A rectal prolapse is where the last part of the rectum or bowel becomes stretched and protrudes (bulging) from the bottom (anus). This could be caused by a weakness of the muscular pelvic floor and ligaments that support your rectum. Sometimes this may only occur when your bowel is opened, and goes back itself.
In more severe cases the rectum may need to be pushed back in after your bowel has been opened, or may even stay outside all the time.
There are 3 types of rectal prolapse:
- Full thickness – protrusion of the full thickness of the rectal wall through the anus.
- Mucosal prolapse – the rectal mucosa (not the entire wall) from the anus.
- Internal prolapse – a part of the intestine which folds into the section next to it.
This could have been caused by:
- age
- chronic constipation
- straining
- pregnancy / child birth
- poor bowel control
- neurological disorders, for example, Dementia
- weakness of the pelvic floor.
What are the symptoms of a rectal prolapse?
Symptoms can include:
- mucus discharge
- bulging on straining
- sensation of incomplete bowel motion
- faecal incontinence
- anal pain
- constipation
- rectal bleeding
How will the operation benefit me?
You have been advised you need surgery to repair your rectal prolapse. This is known as a Delorme’s procedure. The aims of this procedure are to try and repair the prolapse and to prevent it from reoccurring.
Are there any risks or possible complications?
These risks are applicable to any minor or major surgery:
Bleeding. Bleeding from the operation site can happen for up to 1 week. If this bleeding continues and shows no signs of stopping you may need another operation to stop the bleeding.
Risks associated with general anaesthetic. You will be given a leaflet “You and your anaesthetic” which explains in detail about anaesthesia. Your anaesthetist (a doctor with special training in anaesthetics) will discuss this with you.
Deep vein thrombosis – DVT (blood clots in the leg veins) or pulmonary embolism – PE (blood clots in the lungs)
You will be given a leaflet ‘Reducing the risk of a venous thromboembolism (blood clots) while you are in hospital and after you have been discharged’ which explains about this in detail.
All adult patients will have their risk of developing a blood clot assessed within 12 hours of admission. Patients who are being admitted for planned surgery may have their risk assessed at a pre-assessment visit.
The nurse or doctor who carries out the risk assessment will discuss your risk factors with you and advise on treatment to reduce your risk.
You will also be given information, ‘Your personal advice for the prevention of venous thromboembolism (blood clots)’ advising you on how to reduce your risk of developing a blood clot while you are in hospital and when you go home.
Infection. This can be treated with a course of antibiotics and you may need a longer stay in hospital.
Incontinence. You may have some leakage of mucus or faeces after your operation which can cause staining on your underwear. This is due to the gentle stretching of the anus (opening to the back passage) during the operation. This can last for a few weeks and usually needs no treatment. You could wear pant liners.
Recurrence. If this happens you may need further treatment or another operation.
Injury to nearby organs, nerves or tissues. If this happens you may need further treatment or another operation.
Narrowing of the anal canal.
Faecal incontinence. This can be temporary or permanent.
Leaking from the join in the rectum.
Pre-assessment clinic
What will happen at the pre-assessment clinic?
About 2 weeks before your operation, you will be sent an appointment to attend the pre-assessment clinic unless you have already attended after your outpatient appointment.
You will be asked about your general health. Your blood pressure, pulse and weight will be checked. Please remember to bring a fresh sample of your urine with you and all tablets, medicines, inhalers and creams you are using. Your nurse will tell you if you need to stop taking any of these before your operation. Samples of your blood will be taken and you may be sent for x-ray and ECG (a heart tracing).
What do I need to do before the operation?
Bowel preparation is very important before this operation so you might be asked to come in the day before or in the morning of the operation. This will be given by either medication or an enema (medication to empty the bowel). This helps your surgeon to be able to perform the surgery more effectively.
Routine blood tests may have been done in pre-assessment, but if not they will be done before your operation.
You will be given some anti-embolism stockings ‘TED stockings’ to wear before, during and after the operation, this is to help prevent blood clots forming in your legs. After the operation you may be given an injection every day for 4 – 6 weeks which will also help prevent clots after surgery.
Why am I asked not to eat or drink before my operation?
Your nurse will tell you when you must stop eating or drinking before your procedure. This is very important. You must follow the instructions. Nothing means nothing at all, (including water and chewing gum).
If you forget and do eat or drink anything you must tell your doctor or nurse, as your procedure may need to be postponed for your safety. This is because when you are unconscious, if your stomach contains food or drink you may be sick and it could get into your lungs, affect your breathing and cause an infection.
What will happen during my operation?
Your theatre nurse will check your details again before taking you into the anaesthetic room. If it is below 36°C (98.6°F), the procedure will not start until you are warm. A warm air blanket or jacket may be used to raise your temperature.
When in the operating theatre and the recovery room your nurse will take your temperature regularly. If it falls below 36°C (96.8°F), you will be placed under a warm air blanket or jacket.
In the anaesthetic room you will meet your anaesthetist again; a cannula (fine needle) will be placed in the back of your hand or arm so we can inject drugs. Sometimes, when drugs are injected they may feel cold and sting a little.
An intravenous drip may be attached to your cannula. Your blood pressure will be measured. Your pulse will be taken, and the amount of oxygen in your blood will be measured by attaching a special clip to your finger. This does not hurt.
Your heart rate will be monitored by placing sticky pads on your chest. These are attached to some leads to show a tracing of your heart on a monitor. This is routine and is nothing to worry about.
The operation will be carried out under a general anaesthetic (a state of carefully controlled and supervised unconsciousness that means you are unable to feel any pain) or spinal anaesthetic.
The excess lining (Mucosa) is removed from the prolapse to expose the muscle of the bowel wall. The muscle is then stitched to repair the prolapse. This is done via the anus and no external cut is required.
What will happen after the operation?
You will be taken to the recovery room. Specially trained nursing staff will look after you until you are ready to return to your ward.
You will return back to the ward with a catheter (tube into the bladder) until you are able to pass urine without any discomfort. This is usually around 1 – 2 days.
If at any time you are in pain or feel sick, please let one of your nurses know and they will give you medication to help relieve it.
You will have an intravenous drip in your hand or arm through which you will receive fluids to prevent you from dehydrating until you are able to eat and drink normally again.
Patients are encouraged to keep mobile within their ability after the procedure. They should avoid heavy lifting or increased physical activities for 6 weeks.
Will I be able to open my bowels?
Your bowels will have been emptied prior to your operation. The feeling of not wanting to pass any bowel motion may last for a few days.
You may experience a little discomfort and slight bleeding the first few times you empty your bowel. This is normal and can be expected.
You may also pass some mucus from your anus for about 1 week. You may be advised to wear a pad to protect your clothing until these symptoms have settled down.
You should avoid straining when trying to open your bowels. You may be given laxatives to help soften your stools and stimulate (encourage) a bowel motion from the day of your operation.
How long will I be in hospital for?
Every patient is different and recovers at different speeds. We recommend that you stay in hospital until you are reasonably comfortable when passing a motion. This can take up to 3 – 4 days after the operation. It is important to try and be mobile as soon as you feel safe to do so and hygiene is important to try and prevent any infection. You are able to take a shower the day after the procedure
Will I have any sutures (stitches) to be removed?
No. Any sutures used are internal.
How long will I need to be off work?
This may vary from 4 – 8 weeks off after your operation, depending upon the type of work you do. You should ask your doctor or GP for advice. If you are taking any medication that makes you drowsy, you must not drive or operate machinery.
You should try to avoid any lifting that may require straining. Most patients require 2 weeks off work, however every patient is different. You should only do what you feel able to do and give your body time to heal.
If you require a ‘Fit note’ for work please let a member of staff know before you are discharged from hospital.
How will I feel when I go home?
When you go home, if you notice any of the following:
- severe pain in the lower abdomen, rectum or lower back or lower back passage or lower back
- high temperature
- persistent nausea or vomiting
- persistent bleeding from the rectum
You Must contact the specialist colorectal nurse or seek medical help immediately.
How can I help myself?
If you have trouble in controlling your motions or have problems with leakage, this may not improve straight away so give it time. In some cases exercises are given and advice from a specialist colorectal nurse to help with these symptoms.
To help prevent the prolapse returning you should:
- increase the amount of fluid at least 6-8 glasses a day. This can include water, tea, coffee, fruit juice or soup.
- try not to become constipated. You may need to consider taking a fibre supplement, such as Fybogel to help prevent constipation.
- avoid straining.
- take special care not to become constipated if you become pregnant.
You should increase the amount of fibre in your diet gradually as a sudden increase can cause abdominal discomfort and wind. Below are a few examples of the foods you could introduce into your diet.
- Wholemeal bread, pasta and rice
- Beans
- Lentils
- Vegetables and fruit
- Nuts
- Seeds
- High fibre cereals.
When can I drive again?
You can drive 2 weeks after the operation, however, if you do not feel ready to drive then wait until it is safe to carry out an emergency stop.
You should check with your insurance company as policies may vary with individual companies.
When can I play sport again?
You should not go swimming until the area has healed, and only do sport activities if you feel you are up to it.
Will I have a follow up appointment?
You will have a follow up appointment 6 – 8 weeks after the operation. If you haven’t received an appointment please call the outpatient department or the ward which you were discharged from, they will be able to check this for you.
Outpatient Department: 01642 383838
Contact numbers
If you have any worries or concerns during the first 24 hours following your discharge from hospital, please phone the ward to which you were admitted.
After 24 hours; please seek advicefrom your GP.
North Tees and Hartlepool NHS Foundation Trust
University hospital of North Tees
Ward 28
Telephone: 01642 382828
24 hours a day, 7 days a week
Ward 31
Telephone: 01642 382831
24 hours a day, 7 days a week
Day Case Unit
Telephone: 01642 624168
Monday – Friday 8am – 5pm
Specialist Colorectal Nurses
Telephone: 01642 624399
Monday – Friday 9am – 4.30pm
Hospital of Hartlepool
Ward 9
Telephone: 01429 382809
24 hours, 7 days a week
Day Case Unit
Telephone: 01429 522949
Monday – Friday 8am – 5pm
Non-urgent messages can be left on the answering machine
Who do I contact if I need any advice?
Any concerns you may have during the 24 hours following your discharge from hospital, please phone the ward to which you were admitted. After 24 hours; please seek advicefrom your GP
NHS 111 offers medical help and advice from fully trained advisors supported by experienced nurses and paramedics. Available over the phone 24 hours a day contact 111.
NHS choices Provides online information and guidance on all aspects of health and health care, to help you make choices about your health. Website: www.nhs.uk
This patient leaflet is attributed to St Marks Hospital for Colorectal Diseases
Comments, concerns, compliments or complaints
Patient Experience Team (PET)
We are continually trying to improve the services we provide. We want to know what we’re doing well or if there’s anything which we can improve, that’s why the Patient Experience Team (PET) is here to help. Our Patient Experience Team is here to try to resolve your concerns as quickly as possible. The office is based on the ground floor at the University Hospital of North Tees if you wish to discuss concerns in person. If you would like to contact or request a copy of our PET leaflet, please contact:
Telephone: 01642 624719
Freephone: 0800 092 0084
Opening hours: Monday to Friday, 9:30am to 4:00pm
Email: [email protected]
Out of hours
Out of hours if you wish to speak to a senior member of Trust staff, please contact the hospital switchboard who will bleep the appropriate person.
Telephone: 01642 617617
Data protection and use of patient information
The Trust has developed Data Protection policies in accordance with Data Protection Legislation (UK General Data Protection Regulations and Data Protection Act 2018) and the Freedom of Information Act 2000. All of our staff respect these policies and confidentiality is adhered to at all times. If you require further information on how we process your information please see our Privacy Notices.
Telephone: 01642 383551
Email: [email protected]
Privacy NoticesLeaflet feedback
This leaflet has been produced in partnership with patients and carers. All patient leaflets are regularly reviewed, and any suggestions you have as to how it may be improved are extremely valuable. Please write to the Clinical Governance team, North Tees and Hartlepool NHS Foundation Trust, University Hospital of North Tees, TS19 8PE or:
Email: [email protected]
Leaflet reference: PIL1063
Date for Review: 09:02:2025