Information for patients
This leaflet can be made available in other formats including large print, CD and Braille and in languages other than English, upon request.
Your doctor has recommended you have a pacemaker fitted to treat an abnormal heart rate and rhythm.
This leaflet will help you understand what will happen before, during and after the procedure.
How does the heart work?
The heart is a muscle that pumps blood around the body. The heart has its own electrical system that keeps it working and adjusts the heart rate when required.
Some patients develop problems with their heart’s electrical system, sometimes causing an abnormal heart rhythm.
Abnormal heart rhythms can cause symptoms such as shortness of breath, dizziness, blackouts, or if left untreated could cause death in some cases. A pacemaker can help prevent or treat these.
Generally, you will need a pacemaker because your heart is beating too slowly, either all the time or some of the time. The pacemaker will help your heart to beat at a normal rate.
What is a permanent pacemaker?
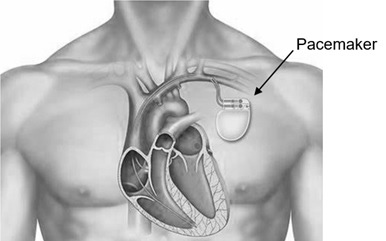
A pacemaker is an electronic device about the size of a small biscuit, protected by a metal casing. When in place, the pacemaker sits under the skin below the collar bone.
It is connected to one or more leads which have been passed along blood vessels in the chest to the heart.
Using these leads the pacemaker constantly monitors the heart’s electrical activity, and can stimulate the heart to beat by sending tiny electrical impulses along the leads to the heart.
Pacemakers work on demand and will only do this when needed.
Many patients feel better and notice an improvement to their quality of life after having a pacemaker.
What should I do before my pacemaker implant?
Your procedure will be performed at the Cardiology Day Unit at the University Hospital of North Tees. You will be sent a letter telling you when and where to come. The pre-assessment nurse will also tell you if you need to stop any medication (drugs) such as anticoagulants or anti-platelets (blood thinners).
All your other medication must be taken as normal and you should bring all your medication with you. The letter will give you instructions on when you should stop eating and drinking.
It is important you arrive at your appointment on time so we can prepare you for your procedure and answer any questions you may have.
We cannot give you a specific time for your procedure as this depends on the needs of all our patients. We will try and keep you fully informed.
Most patients will be discharged on the same day as the procedure, however some patients may need to stay in hospital overnight.
This is to monitor your blood pressure, heart rate, temperature and wound, and for a chest X-ray and pacemaker check to be performed.
Who will be present during my procedure?
A team of healthcare professionals including a cardiologist (a doctor who specialises in conditions of the heart), nurses, cardiac physiologists (a person qualified to perform tests on the heart), and a radiographer (a person qualified to take X-rays and scans).
Trainees may also be present, who will be supervised by fully qualified staff at all times.
North Tees and Hartlepool NHS Foundation Trust is a teaching organisation. We could not train future doctors, nurses or other health professionals without the co-operation of patients.
What will happen when I arrive at the Cardiology Day Unit?
A nurse will show you to a bed in a screened area. You will need to change into a theatre gown and if you wish your own dressing gown.
The information given at your pre-assessment appointment will be checked for changes.
A nurse will check your blood pressure and pulse and insert a cannula (a fine tube) into a vein in your arm or the back of your hand using a small needle. This allows blood samples to be taken and medication to be given before and during the procedure.
A doctor or nurse will explain the procedure and also confirm you have signed a consent form.
What will happen during the procedure?
The procedure takes about 90 minutes. You will lie on a theatre bed with an X-ray machine above it. A nurse will be with you throughout to make sure you are comfortable. You will be given antibiotics to reduce the risk of infection. You will also be offered light sedation to help you relax and ease any anxiety.
You will be connected to equipment to monitor your heart rate, blood pressure and oxygen levels, throughout the procedure. The theatre nurse will clean your upper chest with an antiseptic solution and place sterile drapes under your back and over your chest, leaving a small area exposed for the pacemaker to be implanted.
You will have a local anaesthetic which means you will be awake during your procedure. You will be given additional painkillers and/or strong sedation to reduce any discomfort and make you drowsy.
If at any time during the procedure you feel pain or would like to have more painkillers or sedation, let your nurses or doctor know.
A small incision (cut) will be made below the collarbone and a suitable vein will be found, which is used to pass the lead or leads into the heart. The leads are positioned using X-rays. You may be aware of the X-ray machine moving, it will not touch you. The cardiologist may use a type of X-ray dye, called contrast medium, to identify your veins on X-ray.
You may hear team members talking to each other during the procedure as checks are made to the leads and pacemaker. You may also be asked to take deep breaths or to cough during the procedure. This is all normal and nothing to worry about.
The pacemaker is connected to the lead or leads and placed under the skin in your upper chest, before the wound is closed using dissolvable stitches. A sterile dressing is applied over the wound.
What happens after the procedure?
After the procedure you will return to your bed in the Cardiology Day Unit. We will continue to monitor your blood pressure, pulse, temperature and wound. You will be offered drinks and snacks.
You will have an X-ray and a pacemaker check and we will answer any questions you may have before you are discharged home, or transferred to a ward for overnight stay. You will be given a discharge advice leaflet telling you how to care for your wound where the pacemaker is fitted.
We will make you an appointment for a pacemaker check 4 to 6 weeks after the procedure. We recommend that strenuous activities are avoided until then.
When can I go back to work?
This will depend on your job; you may need at least 1 week off work. This will be discussed with you before you go home.
When can I drive?
If you drive, you must inform the DVLA that you have a pacemaker. You can inform the DVLA using their website. You must also inform your insurance company you have a pacemaker.
If you hold a normal driving licence, you are not allowed to drive for at least 1 week after your pacemaker is fitted.
If you have a Group 2 licence, for example, vocational, HGV or PSV, the DVLA will advise when you can start driving again. If you are a taxi driver, you need to inform your licencing authority.
What are the risks and possible complications?
As with any procedure, complications can occur. You will have an opportunity to discuss these at your pre-assessment. You will be checked for signs of any problems throughout the procedure.
The following are common or important complications:
- Pneumothorax (puncture) of the lung. This can happen to 1 patient in every 100. If this happens you may need a short stay in hospital and another procedure.
- Haemothorax (bleeding into the lung). This is less common than a pneumothorax. If this happens you will need to stay in hospital and may need another procedure. While it doesn’t usually cause problems, it can be life threatening.
- Pericardial effusion (blood leak around the heart). This is rare but can happen to 2 patients in every 1,000. If this happens you may need a short stay in hospital and another procedure.
- Air embolus (air entering a vein). This can happen when the leads are inserted into the vein. Staff follow methods to reduce the risk of this happening.
- Lead displacement. There is a small risk that one of the pacemaker leads may move out of position. This usually needs a further procedure to reposition them.
- Infection. There is a small risk of getting an infection at the site of the pacemaker. You will be given antibiotics at the time of your procedure to help prevent this happening.
- Pain. You may feel a small amount of pain during or after the procedure. Taking painkillers such as paracetamol should help. Always follow the instructions provided in the leaflet supplied with your tablets.
- Conscious light sedation. This can sometimes cause problems with your breathing, heart rate and blood pressure.
- Bleeding, bruising and swelling. There may be some bleeding and bruising to the skin above the pacemaker. This will settle over around 4 weeks.
- Scar. There will be a small scar visible on your chest wall.
- Reaction to the dye (contrast medium). About 1 in every 1000 may have a mild reaction. About 1 in every 40,000 may have a more severe reaction. Contrast will only be used if the cardiologist needs to check the anatomy of your veins on the X-ray camera
- Radiation. The procedure uses ionising radiation (X-rays). Ionising radiation can cause cell damage that may, after many years or decades, turn cancerous. The risk has been carefully compared to the benefit of having the procedure; the benefits of this examination outweigh any small radiation risk.
The risk of this happening is low: it can happen to less than 1 patient in every 10,000 for this procedure. For comparison the above radiation risk represents a very small increase over the natural risk of getting cancer of 1 person in every 2.
It is equivalent to living 1 to 2 months in the UK natural background radiation.
If you think you may be pregnant you must let the staff know as soon as possible before the procedure.
Contact Numbers
If you need further advice, or have any problems, please contact the appropriate number below.
University Hospital of North Tees
Cardiology Day Unit
Telephone: 01429 522020
Monday to Friday, 8.30am to 5.00pm
If no reply leave a message or telephone: 01429 522021
(These are Hartlepool codes but you will be diverted to North Tees.)
Pacemaker Clinic
Cardiac Investigations Unit
Telephone: 01642 624500
Monday to Friday, 9.00am to 5.00pm
Non-urgent messages can be left at any time on the answering machine.
University Hospital of Hartlepool
Pacemaker Clinic
Cardiac Investigations Unit
Telephone: 01429 522249
Monday to Friday, 9.00am to 5.00pm
Non-urgent messages can be left at any time on the answering machine.
The Cardiology Department of North Tees and Hartlepool NHS Foundation Trust run an active research programme of clinical trials. If you are interested, please ask your consultant or nurse if there are any suitable trials to participate in.
Further information is available from:
NHS Choices
Telephone: 111 (when it is less urgent than 999)
Calls to this number are free from landlines and mobile phones
Further information on the NHS Choices website.
British Heart Foundation
Compton House,
2300 The Crescent,
Birmingham Business Park,
Birmingham,
B37 7YE
Telephone: 020 7554 0000
Heart helpline: 0300 330 3311
Monday to Friday, 9.00am to 5.00pm
Further information on the British Heart Foundation website.
Arrhythmia Alliance
P O Box 3697,
Stratford-upon-Avon,
Warwickshire,
CV37 8YL
Telephone: 01789 450 787
24 hours a day, 7 days a week
Further information on the Arrhythmia Alliance website .
References
- Timperley J, Leeson P, Mitchell ARJ, Betts T, 2008, Pacemakers and ICD’s, Oxford specialist handbooks in cardiology, Oxford University Pres
- www.gov.uk/government/publications/ionising-radiation-dose-comparisons/ionising-radiation-dose-comparisons
Comments, concerns, compliments or complaints
Patient Experience Team (PET)
We are continually trying to improve the services we provide. We want to know what we’re doing well or if there’s anything which we can improve, that’s why the Patient Experience Team (PET) is here to help. Our Patient Experience Team is here to try to resolve your concerns as quickly as possible. The office is based on the ground floor at the University Hospital of North Tees if you wish to discuss concerns in person. If you would like to contact or request a copy of our PET leaflet, please contact:
Telephone: 01642 624719
Freephone: 0800 092 0084
Opening hours: Monday to Friday, 9:30am to 4:00pm
Email: [email protected]
Out of hours
Out of hours if you wish to speak to a senior member of Trust staff, please contact the hospital switchboard who will bleep the appropriate person.
Telephone: 01642 617617
Data protection and use of patient information
The Trust has developed Data Protection policies in accordance with Data Protection Legislation (UK General Data Protection Regulations and Data Protection Act 2018) and the Freedom of Information Act 2000. All of our staff respect these policies and confidentiality is adhered to at all times. If you require further information on how we process your information please see our Privacy Notices.
Telephone: 01642 383551
Email: [email protected]
Privacy NoticesLeaflet feedback
This leaflet has been produced in partnership with patients and carers. All patient leaflets are regularly reviewed, and any suggestions you have as to how it may be improved are extremely valuable. Please write to the Clinical Governance team, North Tees and Hartlepool NHS Foundation Trust, University Hospital of North Tees, TS19 8PE or:
Email: [email protected]
Leaflet reference: PIL1085
Date for Review: March 2027