Information for patients
This leaflet can be made available in other formats including large print, CD and Braille and in languages other than English, upon request.
You have had a Percutaneous Endoscopic Gastrostomy (PEG) tube inserted. This leaflet tells you how to care for it, receive feeds through it, and how to manage any problems which may arise.
During your stay in hospital after having your PEG tube inserted your nurses will give you your feeds and care for your tube. You and your carers will be shown how to do this, so by the time you are discharged from hospital you can manage your feeds and care for your tube.
Most people are able to manage their own PEG feeding at home with the help of relatives, carers, district nurses, specialist nurses or their GP. You should contact your district nurse or GP if you need help or advice with your PEG. Your Nutricia Team nurse can visit you in your own home, if needed.
How should I care for my PEG?
The area where the PEG enters your stomach is called the stoma. It is important to keep this area clean and dry to help prevent it becoming infected.
Your specialist nurse will teach you and your carer(s) how to clean and care for your PEG tube and stoma site. You will be given the equipment you need to keep your PEG tube and stoma site clean and healthy.
Before doing anything with your PEG tube, you should always wash and dry your hands.
You must:
check your stoma and surrounding skin every day for signs of redness or leakage. If you have any of these you must contact your district or specialist nurse for advice.
clean and dry your stoma and surrounding skin every day.
turn your tube 360º (one full circle) every day.
flush your tube with water before and after giving feeds or liquid medicine.
contact your specialist nurse, Nutricia Team nurse or GP if your tube or ‘Y’ connector becomes damaged, so arrangements can be made for it to be replaced.
put your special liquid feeds, water or liquid medicines down your PEG tube.
You must not:
put solids or ordinary liquidised foods into your PEG tube.
put any sharp instruments down your PEG tube.
try to repair the tube yourself (your tube may fall out).
cut the tube.
fasten your tube to your clothes with pins.
use talcum powder around your stoma.
First 7 days after PEG placement
One of your nurses will gently clean your stoma and surrounding skin every day.
7 – 28 days after PEG placement
You must clean around your PEG tube every day, using non-perfumed soap and warm water, and rotate (turn) your PEG tube 360º (one full circle) clockwise to keep your stoma healthy.
After 28 days
You must clean around your PEG tube every day using soap and water. The disc which holds the tube against your skin can now be unclipped and moved half way down the tube so you can clean it with cotton buds or a soft toothbrush. Your nurse will teach you how to do this.
Can I have a bath, shower, or go swimming?
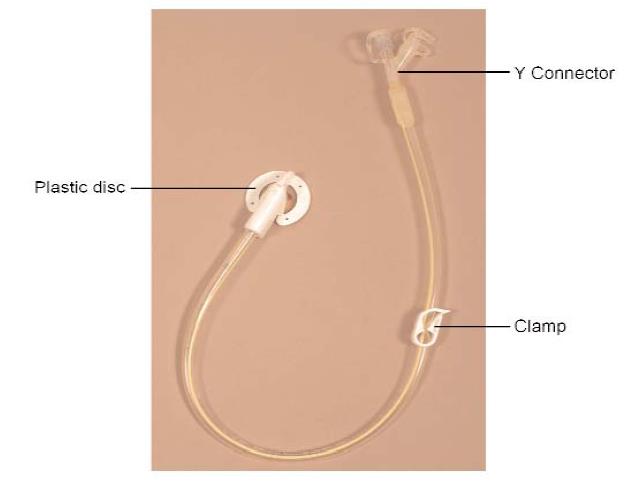
Once your stoma site is healed, usually after 2 weeks, you can bathe, shower or go swimming, but you mustmake sure the ‘Y’ connector openings are closed and your PEG tube is clamped.
How should I care for my mouth and teeth?
You must keep your mouth clean to avoid infection. Daily cleaning of your teeth, including any false teeth, is very important. If you cannot eat and drink normally it is very important to rinse your mouth a few times each day to keep it moist.
How should I give a feed, water or liquid medicines through my PEG?
When a feed, water or liquid medication is given you should be in a sitting position and leaning slightly to the right. This helps prevent reflux (liquids coming back up your oesophagus (gullet) which could cause breathing difficulties or make you feel sick. You should stay in a sitting position for about 30 minutes after a feed to help prevent reflux.
To give a feed, water or liquid medicines you should:
- wash and dry your hands before handling your PEG.
- make sure your PEG tube is above your stoma, pointing towards your chest. This helps prevent the feed from flowing back into the tube, which could cause leakage.
- open the clamp (see diagram).
- take the plunger out of a 50ml syringe.
- attach the syringe to your PEG tube. Pour 30 – 50ml of water into the syringe before giving a feed or medicines to flush (rinse through) your PEG tube. Cold tap water or cool boiled water may be used.
- gently shake your liquid feed bottle before opening.
- remove the seal from the top of the bottle of feed and pour some into the syringe. Repeat this until the full amount of feed prescribed has been given. Your dietitian will tell you how much feed you need to have, and how often each day.
- stop feeding and contact your district nurse, specialist nurse, or GP straight away if there is leakage of fluid from your stoma.
- pour 30 – 50ml of water into the syringe after giving a feed or medicines to flush your PEG tube. Cold tap water or cool boiled water may be used.
- close the clamp
- change the position of the clamp on the tube between feeds or giving medicines to prolong the life of the tube and prevent damage.
- rinse your syringe with warm water after use and leave to dry. A new syringe must be used every day.
If any feed is left in the bottle it must be kept in a fridge and used within 24 hours. After this any left over must be thrown away.
You must not:
- use pins to secure the tube to your clothes.
- ever put anything down your PEG tube other than:
- special liquid feed (as prescribed)
- water
- medicines in liquid form.
You must stop the feed immediately and contact your district nurse or GP immediately if:
- there is any leakage of fluid around your stoma (tube).
- you have pain on feeding.
- there is any new bleeding from your stoma site.
What equipment will I need?
You will be given a 7 day supply of your feeds, syringes and any other equipment you need before you leave hospital. Unopened bottles of your feeds should be stored in a cool, dry place, but not a fridge. If your dietitian advises you need a feeding pump this will be supplied and you and your carer(s) will be shown how to use it. Separate written instructions will be given.
How do I get further supplies?
Your dietitian will inform your GP about your feeds and equipment. Your dietitian will also register you with a feed company’s specialist nurse and home delivery service, if you agree.
You must arrange for repeat prescriptions from your GP.
You can:
- send your first prescription to the home delivery service who will then arrange all future deliveries of your feeds and equipment
or
- take your prescription to your local pharmacy (chemist).
You must always keep at least 7 days supply of your feeds.
What should I do if my PEG tube becomes dislodged or blocked?
PEG tubes last for many months or years, but from time to time the plastic may become damaged and need to be replaced. Replacing a PEG tube is usually a very straightforward procedure.
If your PEG tube becomes dislodged or accidentally removed you must contact your district nurse, specialist nurse, GP or the Emergency Department at your nearest hospital, immediately. Your stoma site will start to close within 2 hours unless a replacement tube is fitted.
If your tube becomes blocked you can try the following:
- make sure the clamp is open.
- make sure the tube is straight and not kinked.
- flush the tube with 25 – 30ml of warm, not boiling, water and leave for 30 minutes, then re-flush.
You must never:
- use too much force.
- try to unblock the tube by putting a solid object or sharp instrument down it. If your tube remains blocked or you are not happy to try and unblock it yourself you must contact your district nurse, specialist nurse or GP straight away.
What help is available after I go home from hospital?
When you go home from hospital you and your carer(s) will have been taught how to give a feed and care for your PEG tube. A number of healthcare professionals are available if you have any problems or concerns and can visit you at home, if needed.
They include:
- district nurses. District nurses are available 24 hours a day, 7 days a week. They can be contacted through your GP’s surgery or NHS 111.
- a specialist nurse.
- a nutritional nurse. Your nutritional nurse is a member of the Hospital to Home service. They work closely with your dietitian and specialist nurse and will visit you in your own home to discuss any problems or concerns you may have. They can also arrange for future deliveries of your feeds and equipment.
- a dietitian. Your dietitian works closely with your district nurse, nutritional and specialist nurses to check your nutritional needs are met.
What will happen if I want to go on holiday?
If you are using the Hospital to Home service they will arrange delivery of your feeds and equipment, free of charge. Always check with your nutritional nurse at least 6 weeks before travelling to check this service is available for where you are going.
There may be a local tax to pay in some countries.
If you get your supplies from your local pharmacy you will have to make your own arrangements.
Contact numbers
If you need further advice, or have any problems, please contact:
University Hospital of North Tees
Department of Nutrition and Dietetics
Telephone: 01642 624768
Monday to Friday, 9.00am to 4.00pm
Specialist nurses
Telephone: 01642 624682
Monday to Friday, 9.00am to 5.00pm
Endoscopy Unit
Telephone: 01642 624387
Monday to Saturday 8am to 7pm
Nutricia Nutritional nurse
Telephone: 08457 623654
Monday to Friday, 9.00am to 5.00pm
Outside these hours please contact Nutricia Nutritional nurse advice line telephone: 08457 623636.
Emergency Department
Telephone: 01642 382899
24 hours a day, 7 days a week
If you have any worries or concerns you should contact your GP during normal surgery hours. Outside surgery hours, you should contact NHS 111.
Further information is available from:
NHS Choices
Telephone: 111 (when it is less urgent than 999)
Calls to this number are free from landlines and mobile phones
or via the website at www.nhs.uk
Comments, concerns, compliments or complaints
Patient Experience Team (PET)
We are continually trying to improve the services we provide. We want to know what we’re doing well or if there’s anything which we can improve, that’s why the Patient Experience Team (PET) is here to help. Our Patient Experience Team is here to try to resolve your concerns as quickly as possible. The office is based on the ground floor at the University Hospital of North Tees if you wish to discuss concerns in person. If you would like to contact or request a copy of our PET leaflet, please contact:
Telephone: 01642 624719
Freephone: 0800 092 0084
Opening hours: Monday to Friday, 9:30am to 4:00pm
Email: [email protected]
Out of hours
Out of hours if you wish to speak to a senior member of Trust staff, please contact the hospital switchboard who will bleep the appropriate person.
Telephone: 01642 617617
Data protection and use of patient information
The Trust has developed Data Protection policies in accordance with Data Protection Legislation (UK General Data Protection Regulations and Data Protection Act 2018) and the Freedom of Information Act 2000. All of our staff respect these policies and confidentiality is adhered to at all times. If you require further information on how we process your information please see our Privacy Notices.
Telephone: 01642 383551
Email: [email protected]
Privacy NoticesLeaflet feedback
This leaflet has been produced in partnership with patients and carers. All patient leaflets are regularly reviewed, and any suggestions you have as to how it may be improved are extremely valuable. Please write to the Clinical Governance team, North Tees and Hartlepool NHS Foundation Trust, University Hospital of North Tees, TS19 8PE or:
Email: [email protected]
Leaflet reference: PIL1007
Date for Review: March 2027