Information for patients
This leaflet can be made available in other formats including large print, CD and Braille and in languages other than English, upon request.
Introduction
This leaflet aims to provide information about mechanical thrombectomy as treatment of ischaemic stroke, including the benefits, risks and what to expect when you undergo this procedure. If you have any further questions, please speak to the doctor or nurse caring for you.
What is Ischaemic Stroke?
An ischaemic stroke occurs when an artery (blood vessel) is blocked by a clot, cutting off the blood and oxygen supply to that part of the brain. Without adequate blood supply, brain cells lose function and eventually die.
What is mechanical thrombectomy (clot retrieval)?
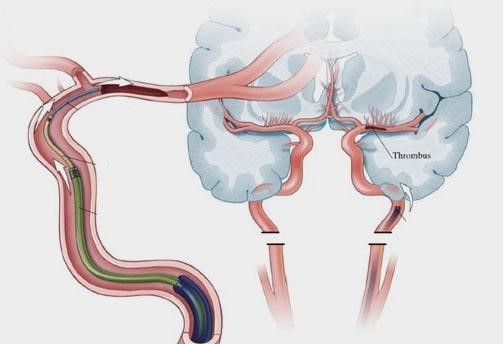
Thrombectomy is an emergency procedure performed by a specialist team led by a doctor called an Interventional Neuroradiologist.
The doctor uses specialised equipment and guidewires to physically remove the clot from the artery in the brain in order to restore the blood supply. If mechanical thrombectomy is not feasible, there is no known better alternative treatment to remove or dissolve the clot. If untreated, the patient’s stroke symptoms can get worse.
What is thrombolysis?
Clots may occur in various parts of the brain. If a clot is blocking a major vessel in the brain, thrombolysis is done in conjunction with thrombectomy.
Thrombolysis is a treatment that uses a strong “clot busting” medication, known as a thrombolytic agent. This is administered through a needle in the vein (venflon) in an attempt to dissolve the clot that blocks the supply of blood.
Thrombolysis is a time critical treatment and must be started as soon as ischaemic stroke symptoms are observed. Thrombolytic agents are known to be most potent when it is given within 3 – 4.5 hours after the onset of symptoms.
There are also risks associated with thrombolysis and not all stroke patients can undergo this treatment. Special care is observed and may be unsuitable to those who have higher risk of bleeding (e.g. those who are on anticoagulant therapy such as Warfarin, Apixaban, Rivaroxaban etc.).
If thrombolysis is not feasible due to known risk factors, then mechanical thrombectomy alone may be considered.
Why am I being transferred to a tertiary hospital?
Mechanical Thrombectomy is a procedure performed by a specialist team. This service is currently not being offered in North Tees Hospital for the reason that the trust do not have the specialist team called Interventional Neuroradiologists on site so it is vital to transfer suitable patients to tertiary hospitals such as Royal Victoria Infirmary. James Cook hospital offers this service as well.
Normally, patients who are suitable for thrombectomy are being discussed with neurosurgeons in either James Cook or Royal Victoria. They then assess the case, consider risks and benefits then make a decision whether to go ahead for the procedure or not. As soon as Neuroradiologist accept patients, the stroke team in North Tees will then facilitate an ambulance transfer to the accepting hospital for the procedure.
What happens during mechanical thrombectomy?
- An incision into the femoral artery in the groin is made and a thin plastic tube (guidewire) is inserted.
- An X-ray detectable contrast dye is injected to better visualise the blood vessels which supply up to and into the brain.
- An X-ray scanner then monitors the highlighted blood vessels and helps guide the route of the catheter up to the brain, and towards the artery which is blocked by the blood clot.
- Once the blockage is reached, a clot-removal device is placed through the catheter tube to take the clot out. A special equipment such as a small wire mesh (stent retriever) or suction devices is used to remove the blood clot and restart blood flow to the affected part of the brain.
In about 7 out of 10 eligible cases, the procedure opens the artery. Occasionally, it may not be possible to get to or remove the clot.

What are the benefits of mechanical thrombectomy?
Undergoing this procedure gives a little less than fifty percent chance of regaining independence. The sooner it is performed the better the chance of recovery, including greater chance of functional independence and mobility.
More than four out of ten patients who undergo thrombectomy will benefit through having less disability over those who did not.
There is no assurance that everyone will completely recover after treatment because the severity of the damage depends on how long the clot blocked the blood supply in the brain. The sooner the clot is removed, the lesser injury is expected and the higher the chances of recovery.
What are the risks of mechanical thrombectomy?
As with any procedure, there are risks associated with thrombectomy, but overall the potential benefits outweigh the potential risks.
- The contrast dye carries a small risk of allergic reaction, and although rare, can temporarily affect kidney function in one out of 20 patients (unless you have predisposing risk factors).
- There is also a minimal risk of bruising, swelling, infection or bleeding in the groin (puncture site). Also, a very few isolated cases are referred to surgery following thrombectomy to repair the artery in the groin. This is done to prevent the circulation in the leg being affected).
- There is also a low risk of bleeding in the brain, which can lead to disability or death.
- There is a very small probability of tearing the artery or re-blockage of the artery, which may lead to disability or death.
- There is also a slight chance that the brain may swell which would further require a major surgery.
What happens after mechanical thrombectomy care?
The nurses will check your observations such as blood pressure, heart rate, oxygen levels and consciousness level. The staff will also monitor your groin and check the pulses in your feet in the first 24 hours after the procedure. You will need to remain on bedrest for four hours as advised by the interventional radiologist. This will help prevent any complications to the groin. Intermittent pneumatic compression stockings are usually applied to help prevent clots forming in the legs (deep vein thrombosis) whilst you are in hospital and less mobile.
You will have a repeat CT head scan after 24 hours to rule out any possibility of complications after the procedure. If the CT scan does not show any signs of bleeding in your brain then you will be started on a medication called Aspirin or similar medications to reduce the risk of any further blood clots.
Why will I be transferred back to my local hospital?
You will be transferred back to your local stroke unit by an ambulance. The transfers usually happen either on the same day, or on the day following the procedure. However, some patients may need ongoing monitoring at the comprehensive stroke centre in Newcastle upon Tyne for a longer period.
Once back at your local stroke unit, you will receive ongoing stroke rehabilitation and follow up in the hospital closest to your home.
Further Information Available
We hope this information sheet has been helpful to you but it is by no means a replacement for talking to either the stroke doctor or a stroke nurse.
Please ask questions if you feel that you need more information.
Stroke Unit
24 hours a day, 7 days a week
Telephone: 01642 382741
NHS Choices
Calls to this number are free from landlines and mobile phones
When it is less urgent than 999 call 111
Website: www.nhs.uk
Useful Websites
If you would like to find accessibility information for our hospitals, please visit www.accessable.co.uk
The Stroke Association also has useful information on their website at www.stroke.org.uk
References/ Further Reading
Kavelin Rumalla, Malte Ottenhausen, Peter Kan and Jan-Karl Burkhardt (2019), Recent Nationwide Impact of Mechanical Trombectomy on Decompressive Hemicraniectomy for Acute Ischemic Stroke. AHA Journals, Volume 50 Number 8. [Last accessed: 30th January 2023]
https://www.ahajournals.org/doi/10.1161/STROKEAHA.119.025063
Ulf Neuberger, Philipp Kickingereder, Silvia Schönenberger, Simon Schieber, Peter A Ringleb, Martin Bendszus, Johannes Pfaff, Markus A Möhlenbruch (2019). Risk factors of intracranial haemorrhage after mechanical thrombectomy of anterior circulation ischemic stroke. National Library of Medicine, Neuroradiology. 61(4):461-469. Last accessed: 30th January 2023] https://pubmed.ncbi.nlm.nih.gov/30778621/
Li H, Huang J, Ye S on behalf of the DIRECT-MT investigators, et alPredictors of mortality in acute ischemic stroke treated with endovascular thrombectomy despite successful reperfusion: subgroup analysis of a multicentre randomised clinical trialBMJ Open 2022;12:e053765. doi: 10.1136/bmjopen-2021-053765. [Last Accessed: 30th January 2023] https://bmjopen.bmj.com/content/12/3/e053765
Additional Information
This leaflet has been adapted from the Royal Victoria Hospital. Information within this leaflet was produced by Dr. Akif Gani (Stroke Consultant), Dr Anand Dixit (Stroke Consultant), Professor Phil White (Interventional Neuroradiologist), Rachel Seal (Stroke Nurse Practitioner), and Laurie Giraldo (Stroke Nurse Practitioner) at the Royal Victoria Hospital and has been adapted for use at University Hospital of North Tees and Hartlepool Foundation Trust.
Comments, concerns, compliments or complaints
Patient Experience Team (PET)
We are continually trying to improve the services we provide. We want to know what we’re doing well or if there’s anything which we can improve, that’s why the Patient Experience Team (PET) is here to help. Our Patient Experience Team is here to try to resolve your concerns as quickly as possible. The office is based on the ground floor at the University Hospital of North Tees if you wish to discuss concerns in person. If you would like to contact or request a copy of our PET leaflet, please contact:
Telephone: 01642 624719
Freephone: 0800 092 0084
Opening hours: Monday to Friday, 9:30am to 4:00pm
Email: [email protected]
Out of hours
Out of hours if you wish to speak to a senior member of Trust staff, please contact the hospital switchboard who will bleep the appropriate person.
Telephone: 01642 617617
Data protection and use of patient information
The Trust has developed Data Protection policies in accordance with Data Protection Legislation (UK General Data Protection Regulations and Data Protection Act 2018) and the Freedom of Information Act 2000. All of our staff respect these policies and confidentiality is adhered to at all times. If you require further information on how we process your information please see our Privacy Notices.
Telephone: 01642 383551
Email: [email protected]
Privacy NoticesLeaflet feedback
This leaflet has been produced in partnership with patients and carers. All patient leaflets are regularly reviewed, and any suggestions you have as to how it may be improved are extremely valuable. Please write to the Clinical Governance team, North Tees and Hartlepool NHS Foundation Trust, University Hospital of North Tees, TS19 8PE or:
Email: [email protected]
Leaflet Reference: PIL1406
Date for Review: 14/12/2025
