Information for patients
This leaflet can be made available in other formats including large print, CD and Braille and in languages other than English, upon request.
Introduction
This leaflet explains why you have been referred for a total hip replacement operation.
The orthorpaedic team are here to assist you with all of your needs, and we will provide you with advice and guidance.
Please contact the team if you have any questions or concerns.
What is a hip replacement?
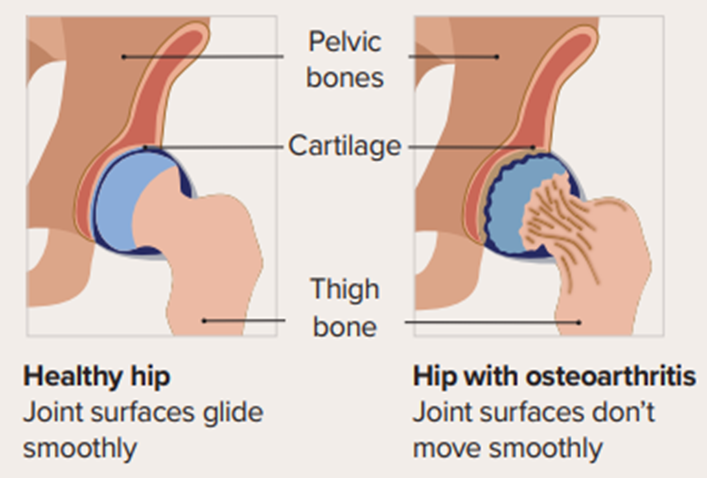
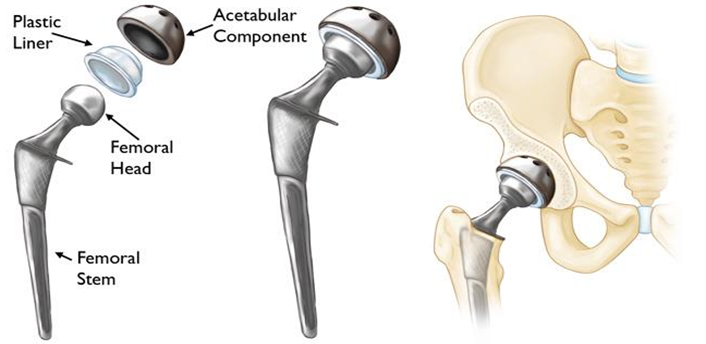
The hip is a ball and socket joint, between the pelvis and the thigh bone. The upper end of the thigh is the ball part and fits into the socket in the pelvis. During the operation, the worn or damaged joint will be replaced with an artificial joint.
What are the advantages of a hip replacement?
A hip replacement is usually carried out because of severe pain and restricted mobility. A hip replacement may provide benefits such as:
- Reduced pain
- Reduced stiffness
With a combination of reduced pain and stiffness, your overall mobility is likely to be improved. This helps you to return to a fitter and more active lifestyle.
What are the associated risks?
Hip replacements are generally very successful, and a high proportion of patients can gain an improved lifestyle benefit. There is, however, a risk of complications. These can include:
What if I need help at home?
You can discuss this with the occupational therapist, who can arrange for carers to be put in place for your discharge.
You will also be given a form on your final check appointment before surgery that will ask you questions regarding equipment that may be needed for your return home, this will all be explained to you by the joint replacement specialist nurse.
Your equipment will be delivered prior to your operation.
How should I prepare for my admission to hospital?
Please ensure you have a bath or shower before you arrive at the hospital to aid in the prevention of the risk of infection.
It is also important that you do not apply creams or make up after your bath or shower. Please do not shave your legs for at least 3 weeks prior to your operation.
Shaving is known to increase infection rates in joint replacement. It is not known whether hair removal creams increase infection risks so these are best avoided.
What should I bring to hospital for my admission?
You should bring well fitting, comfortable slippers or flat supportive shoes to walk in. New slippers may not fit if your feet become swollen, and slippers/shoes without a back are not recommended.
You should also bring easy fitting clothes.
You must bring any other medication normally prescribed by your own doctor, or any over the counter medication with you on admission. Please bring them in their original packets. any medication that is not in its original pack cannot be used on the ward.
Please bring in any leaflets, walking aids, and equipment provided to you for the operation. For example, a helping hand, shoe horn, or sock aid.
Please only bring in essential as there is limited space and no suitable storage for valuables.
What happens during my admission to hospital?
You will be admitted to hospital on the day of your procedure and given a time slot, which is designed to make your stay in hospital before the operation as short as possible.
You will be admitted to the access lounge, where all of the checks will be completed before you go into the theatre.
When you are admitted to the access lounge you will be seen by an anaesthetist, who will discuss your anaesthetic choices with you. Most patients will be recommended to have a spinal anaesthetic, in combination with a light general anaesthetic or sedation.
The spinal anaesthetic involves a small injection of local anaesthetic between the bones of the lower part of the back, around the nerves of the spinal cord.
This causes a temporary numbness and heaviness from the waist down and allows surgery to proceed without you feeling any pain.
Light general anaesthesia or sedation may the be given to reduce your awareness of theatre activity during surgery. This anaesthetic combination is preferred because it is safe, effective and its full effects usually wear off very quickly following surgery.
This allows most patients to make a rapid recovery with few hangover side effects. It will also allow and promote early mobilisation.
Other anaesthetic choices include: general anaesthesia and/or combined with nerve block or epidural anaesthetic. An epidural anaesthetic is similar to a spina anaesthetic, but it can be continued after the surgery in the ward. You anaesthetist will discuss the pros and cons of these choices with you.
From the start of the anaesthetic until the end of your operation, your anaesthetist will stay with you watching your condition very closely. Your heart rate, blood pressure and breathing are monitored throughout and your body temperature is kept normal using a warming blanket.
As with all anaesthetic techniques, there is the possibility of side-effects or complications with a spinal anaesthetic.
Common side effects include:
Rare side effects:
What happens during the operation?
You should be aware that in theatre the operating team wear specialist clothing, hoods and masks. This is to further minimise the risk of infection.
At the end of the operation, the surgeon will inject local anaesthetic into the tissues around the new joint which will assist to relieve your pain.
What happens following the operation?
You will go into the recovery unit. The staff will check your general condition, take observations of your pulse, blood pressure, temperature, oxygen levels (vital signs), check your wound, monitor the reversals of your spinal anaesthetic, and assess if you need any further pain relief.
Once the anaesthetist is happy with your recovery and vital signs, you will return to the ward where the staff will continue to monitor your vital signs, bladder and bowel function, the return of feeling in your legs and lower body following the spinal anaesthetic.
You will have regular pain relief prescribed.
If you feel your pain relief is inadequate at any time then you must let the ward nurses know so that they can help you get more comfortable, and provide you with medication required.
During your stay on the ward you may be seen by the pharmacy team. They will discuss any new medication with you and give you advice on how to take the medicine and the potential side effects you may experience.
Your stay in hospital will be short.
You will be encouraged to attend to your own personal hygiene with minimal assistance and be encouraged to be as independent as possible, you will be expected to get dressed into your normal clothes.
You will be visited by a physiotherapist/occupational therapist daily on the ward.
Continuing with your physiotherapy exercises, and learning how to walk with a Zimmer frame is important before progressing to elbow crutches or walking sticks. You will also practice stair climbing if necessary.
It is important that you exercise independently at times throughout the day when the physiotherapist is not attending you.
You will be escorted to X-ray to have imaging taken of your hip replacement. Blood tests will also be taken on this day.
The nursing staff will discuss your discharge plan with you as soon as possible after your operation, to ensure you have all of the necessary equipment and help in place at home before you leave the ward.
You will be discharged home when you are medically fit and have completed all of your physiotherapy and occupational therapy assessments.
Before you leave the ward you will be given a discharge letter. This contains information about your operation and medication. Your GP will receive a copy of this letter on email on the day you are discharged.
Will my medication change following surgery?
You will be prescribed some new medicines. Some are to help to reduce the amount of pain, and some help to reduce the risks of complications following surgery. There may also be some temporary changes to your regular medicine, but if there are it will be explained to you.
The nursing staff will give you your medication prior to you leaving the ward. You will be discharged from hospital with a 7 day supply of tablets to relieve the pain, and you will need to contact your GP for any further prescriptions required.
You and your GP will be given a copy of your discharge letter.
Movement following surgery
Physiotherapy
It is important to continue with the exercises you were given in hospital. Keep doing the until you see your joint replacement nurse, practitioner or consultant. Depending on where you live you may be given a physiotherapy outpatients appointment after discharge for you to attend.
What happens following discharge home?
A few days after you have been discharged, you will be contacted by a member of the joint replacement specialist nurses to see how you are getting on.
Your wound review appointment will be carried out approximately 2 weeks after surgery, this will be given to you at your pre-operative appointment prior to your operation.
You will have a consultant or joint replacement specialist nurse review around 6 to 8 weeks after surgery to check your progression and discuss hip precautions.
You will be reviewed again 5 months in a virtual clinic (phone call appointment), and asked to attend for an X-ray at your own convenience.
There will be another review at 1 year and asked to attend for an X-ray. If you have met all required milestones you will then be discharged back to the care of your GP.
If you have any concerns regarding your recovery, or think you may be developing a problem please contact the helplines (contact numbers in the back of this booklet). We will be able to offer advice and arrange additional support, or organise a review if required.
How to care for your wound?
Your wound may leak slightly into your dressing and dry up. This is normal, if it leaks outside of the dressing you must contact the service on the number provided.
Your wound dressing should remain in place for at least 14 days, the specialist nurse will give you a return appointment for wound/dressing check review.
Your dressing will only be changed if the dressing will not stay in place or attach to your skin or there is an issue with the wound.
Please do not change the dressing yourself.
The dressing on your hip wound has a bacterial barrier to help reduce the risk of infection, it is not advisable to shower for at least 14 days after surgery. Washes only are advised.
An infection at the site of your wound is unusual but may present as discharge from the wound, redness, swelling and heat, increased pain or an offensive smell. You must seek advice from the helpline number or contact the ward where you had your surgery.
If you are concerned about your wound, please call the helpline at any time.
If your GP or district nurse prescribes antibiotics for a possible wound infection, please contact the joint replacement specialist nurses or ward, we may need to arrange an appointment with your surgeon.
Seek advice from your hospital or GP if you notice any excessive bleeding, or any difficulty with breathing. If you become urgently unwell, call 999 and request an ambulance.
Frequently Asked Questions
References
- NICE (The National Institute for Health and Care Excellence)
- NJR (National Joint Registry)
- Journal of Orthopaedic Surgery and Research
www.josr-online.biomedcentral.com
Contact Numbers
Joint Replacement Specialist Nurses
Monday to Friday, 8:30am to 4:30pm
Hartlepool
01429 522493
Ward 4 Hartlepool
01642 382804
Physiotherapy Ward 4 Hartlepool
01429 522030
Ward 32 North Tees
01642 382732
Ward 33 North Tees
01642 382733
Returning equipment:
Durham and surrounding districts
(01325) 524531
TCES Equipment Hartlepool, Stockton and Middlesbrough
(01642) 224205
Comments, concerns, compliments or complaints
Patient Experience Team (PET)
We are continually trying to improve the services we provide. We want to know what we’re doing well or if there’s anything which we can improve, that’s why the Patient Experience Team (PET) is here to help. Our Patient Experience Team is here to try to resolve your concerns as quickly as possible. The office is based on the ground floor at the University Hospital of North Tees if you wish to discuss concerns in person. If you would like to contact or request a copy of our PET leaflet, please contact:
Telephone: 01642 624719
Freephone: 0800 092 0084
Opening hours: Monday to Friday, 9:30am to 4:00pm
Email: [email protected]
Out of hours
Out of hours if you wish to speak to a senior member of Trust staff, please contact the hospital switchboard who will bleep the appropriate person.
Telephone: 01642 617617
Data protection and use of patient information
The Trust has developed Data Protection policies in accordance with Data Protection Legislation (UK General Data Protection Regulations and Data Protection Act 2018) and the Freedom of Information Act 2000. All of our staff respect these policies and confidentiality is adhered to at all times. If you require further information on how we process your information please see our Privacy Notices.
Telephone: 01642 383551
Email: [email protected]
Privacy NoticesLeaflet feedback
This leaflet has been produced in partnership with patients and carers. All patient leaflets are regularly reviewed, and any suggestions you have as to how it may be improved are extremely valuable. Please write to the Clinical Governance team, North Tees and Hartlepool NHS Foundation Trust, University Hospital of North Tees, TS19 8PE or:
Email: [email protected]
Leaflet reference: PIL1463
Date for Review: September 2026