Information for patients
This leaflet can be made available in other formats including large print, CD and Braille and in languages other than English, upon request.
This leaflet will tell you what an Endoscopic Sleeve Gastroplasty is, and what to expect before and after your surgery.
What is an Endoscopic Sleeve Gastroplasty?
Endoscopic Sleeve Gastroplasty (ESG) is a procedure (operation) which uses an endoscope (a thin, flexible tube with a camera), guided by your surgeon, which will help with weight loss by reducing the size of your stomach.
You will be left without incisions or scars unlike other surgeries. This is explained in more detail further on in the leaflet. The ESG changes the shape of your stomach into a sleeve-like structure.

How is an Endoscopic Sleeve Gastroplasty performed?
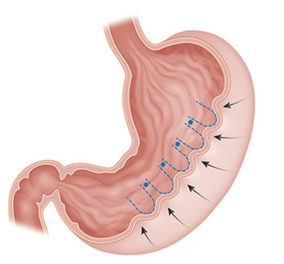
The ESG uses an endoscopic technique which involves a camera, and a small suturing (stitching) device. The suturing device attaches to the camera which is then passed through your mouth into the stomach while you are asleep.
Endoscopic procedures are considered very safe and less risky than a more invasive operation.
The suturing device is then used to create an accordion effect or curtain like folds into the stomach to make it smaller and decrease its size. When these folds are stitched into your stomach tissue, there is less room in your stomach. With a smaller stomach, you should feel fuller faster, tend to eat less food and as a result lose weight.
What Is the expected amount of Weight Loss following an ESG procedure?
Patients who have the ESG weight loss procedure lose on average 49% of excess body weight 12 months after the procedure.1
Is the ESG procedure permanent?
The sutures used in the procedure are made of a durable, permanent material that does not dissolve. Over time, scarring helps maintain the size and sleeve-like shape. In the event the sutures break, or the sleeve stretches, retightening may be performed by your doctor.
Benefits of the ESG procedure
- A Lower Risk procedure – The risk of complications from the Endoscopic Sleeve Gastroplasty procedure are lower than the risk of complications with other surgical procedures. This is because the Endoscopic Sleeve Gastroplasty does not involve incisions or staple lines that could potentially bleed or leak. The procedure takes a shorter time to complete which also contributes to the reduction in risks.
- Fast Recovery – The recovery following the Endoscopic Sleeve Gastroplasty is faster as there are no incisions in the tummy wall.
Are there any risks or possible complications with having an Endoscopic Sleeve Gastroplasty?
As with any procedure there are some risks. These can vary depending on your age and other illnesses you may have. These can include:
- Risks linked with anaesthesia – Your anaesthetist will discuss this with you, when you are pre-assessed for surgery and direct you to further information if necessary.
- Perforation – With any endoscopy (camera examination), there is a very small risk of perforation. Stomach rupture is extremely rare, unless you have had previous gastric surgery.
- Stomach ulcer – To reduce the risk of a stomach ulcer, (painful sore in the lining of your stomach) we prescribe anti-ulcer tablets, and we write to your GP asking these to be continued. You must not stop taking this medication unless; you have been advised by the bariatric team.
Some complications can develop a long time after your ESG procedure.
These can include:
Excess Skin – Following the ESG Procedure as you lose weight you may develop loose skin.
To remove this you may need plastic surgery. If excess skin is developed, you may need to contact your GP for further management.
Rapid weight loss or weight gain – If you do not follow the dietary and exercise advice given you may lose too much weight or you may put weight back on.
What will happen at the Pre-Assessment Clinic?
You will meet the Nurse Practitioner who will answer any questions you may have about your general anaesthesia. The Nurse will complete your admission forms and start to discuss and plan your discharge from hospital after your operation.
Some routine health checks will be taken at the clinic. These will include blood and urine tests, ECG – electrocardiogram (heart tracing), and X-rays if needed.
This reduces the length of time you will need to stay in hospital as an inpatient. You can expect your appointment to last between 1 to 3 hours depending on what tests and checks need to be done.
What do I need to bring with me?
Please make sure you bring socks and slippers, a dressing gown, a vest or other warm clothing to help you feel warm while you are in hospital.
Please arrange for someone to collect your clothing and any items you will not need while you are in hospital, as storage space on the wards is limited.
Please bring in any new medicines your Doctor may have started after your pre-assessment visit. If doses of any other medicines change after your pre-assessment visit, you must tell your Nurse or Doctor when you are admitted.
Please make sure you bring your CPAP machine into hospital with you if you suffer from obstructive sleep apnoea (a condition where the walls of the throat relax and narrow during sleep). This means you stop breathing for short periods of time and use a Continuous Positive Airway Pressure (CPAP) machine.
What will happen while I’m in Hospital?
On admission to the ward, you will be introduced to your ‘named Nurse’, who is responsible for planning your nursing care with you. Your named Nurse is part of a team of Nurses who are there to help and advise you and to make your stay as comfortable as possible.
What will happen before my procedure?
When you arrive, one of the Nurses who will care for you will welcome you to the Access Lounge. They will re-check your details and record your observations (blood pressure, pulse, temperature, etc.).
You will be seen by one of your Doctors, who will tell you the approximate time of your procedure and answer any questions you may have.
Before your procedure, one of your Doctors will again explain the reasons for your operation, the operation itself, and the precautions we take to avoid any risks or complications.
When you fully understand the procedure, you will be asked to sign a consent form, if you have not already done so.
You will be asked to remove any jewellery you are wearing (except your wedding ring), contact lenses, make-up and nail varnish. You will also be advised not to use any body lotions, deodorants and perfumes. You will be asked to put on a theatre gown.
False teeth, glasses and hearing aids may be removed in the operating theatre.
Just before the time of your procedure, one of your Nurses from the ward will go with you and transfer your care to a theatre Nurse.
If you have any worries or concerns, you should tell the staff. They are there to help and support you.
Why am I asked not to eat or drink before my procedure?
Your Nurse will tell you when you must stop eating and drinking before your procedure. This is very important. You must follow the instructions. Nothing means nothing at all, (including water and chewing gum).
If you forget these instructions and you do eat or drink anything, you must tell your Doctor or Nurse, as your procedure may need to be postponed for your safety.
This is because when you are unconscious, if your stomach contains food or drink, you may be sick and it could get into your lungs, affect your breathing and cause an infection.
What will happen during my procedure?
Your theatre Nurse will check your details again before taking you into the anaesthetic room. If it is below 36°C (98.6°F), the procedure will not start until you are warm. A warm air blanket or jacket may be used to raise your temperature.
When in the operating theatre and the recovery room, your Nurse will take your temperature regularly. If it falls below 36°C (96.8°F), you will be placed under a warm air blanket or jacket.
In the anaesthetic room, you will meet your Anaesthetist again. A cannula (fine needle) will be placed in the back of your hand or arm so that drugs can be injected. Sometimes, when drugs are injected, they may feel cold and sting a little.
- An intravenous drip may be attached to your cannula, but this usually takes place when you are anaesthetised.
- Your blood pressure will be measured.
- Your pulse will be taken and the amount of oxygen in your blood will be measured by attaching a special clip to your finger. This does not hurt.
- Your heart rate will be monitored by placing sticky pads on your chest. These are attached to some leads to show a tracing of your heart on a monitor. This is routine and is nothing to worry about.
A checklist will be gone through by the theatre staff to see if it is safe to proceed with the procedure, if it is safe the procedure will be done as discussed previously in the leaflet.
What will happen after my procedure?
You will be taken to the recovery room. Specially trained nursing staff will look after you until you are ready to return to your ward.
How will I feel after my procedure?
You may experience discomfort and nausea. Medication will be given through the cannula in your arm to ease this discomfort. You will receive fluids through this for up to 24 hours to prevent you from dehydrating, until you are able to drink normally.
If at any time you feel sick, please let one of your Nurses know and they will give you medication to relieve it. You will continue to be on a liquid diet for 4 to 6 weeks after your procedure.
How long will I stay in hospital?
You will be discharged home when you are able to drink without any problems. This is usually 1 to 3 days after your procedure.
Discharge Home
Most patients typically go home the next day and return to work in 2 weeks. Your doctor may prescribe you medications to take after the procedure to manage any discomfort you may have or any symptoms that occur.
This will be a medication such as Lansoprazole, to help reduce the production of acid. You will need to take this for 2 years following your procedure, and then this will be reviewed.
When can I eat after my procedure?
Your doctor will tell you when you can eat. When you do eat, it is important to aim for a healthy, well-balanced diet.
Will I need a follow-up appointment?
You will receive a telephone call the week after your discharge to check how you feel. About 6 to 8 weeks following your procedure, you will have an outpatient appointment to check your progress. You will then receive regular appointments with the Bariatric Team for two years following your procedure.
After the first month
With less room in your stomach, you should feel full faster and continue to lose weight. The procedure helps you develop better eating habits and change your lifestyle for lasting results.
What are the common side effects after an ESG procedure?
The most common side effects are gastrointestinal symptoms such as nausea, abdominal pain, vomiting, constipation, burping or diarrhoea. These symptoms typically resolve within 30 to 60 days.
How much fluid should I be drinking?
Drinking plenty of fluid is very important after the ESG procedure. Fluid prevents dehydration and can help prevent constipation.
How much food should I be eating?
Your diet will be as per the diet sheet provided. If you have any problems, you should contact your Dietitian or Bariatric Nurse Specialist.
What should I do if I think I am constipated?
You should make sure you are drinking enough fluids. Your bowels should be opening approximately twice per week. If you have any problems, you should contact your Dietitian or Bariatric Nurse Specialist.
How soon can I start exercising?
Usually when you feel able to do so, you can start gentle exercise. If you suffer from joint pain, taking Non-Steroidal Anti-Inflammatory Drugs (NSAIDS) such as Naproxen, Ibuprofen and Diclofenac should be avoided. If you have any problems, you should contact your Bariatric Nurse Specialist.
When can I drive?
You may drive as soon as you feel comfortable wearing a seatbelt and are able to carry out the emergency stop. You should check with your insurance company for their advice on driving.
How soon can I return to work?
You will be given a 2 week fit note and can return to work following this if you are up to it, if not you should contact your GP.
Contact Numbers
If you need further advice or have any problems, please contact the appropriate number below:
North Tees and Hartlepool NHS Foundation Trust
Bariatric Nurse Specialist
Telephone: 01642 624601
Monday to Friday, 9.00am to 5.00pm
Dietitian
Telephone: 01642 383728
Monday to Friday, 9.00am to 5.00pm
Ward 31
For the first 7 days after hospital discharge only
Telephone: 01642 624592
24 hours a day, 7 days a week
Consultant’s secretary
Telephone: 01642 383292 or 01642 383290
Monday to Friday, 9.00am to 5.00pm
Further information is available from:
The NHS website at www.nhs.uk
References
- Dayyeh, B.A., et.al (2022), Endoscopic sleeve gastroplasty for treatment of class 1 and 2 obesity (MERIT): a prospective, multicentre, randomised trial, The Lancet, Volume 400, issue 10350, P441-451
Comments, concerns, compliments or complaints
Patient Experience Team (PET)
We are continually trying to improve the services we provide. We want to know what we’re doing well or if there’s anything which we can improve, that’s why the Patient Experience Team (PET) is here to help. Our Team is here to try to resolve your concerns. The office is based at the University Hospital of North Tees if you wish to discuss concerns in person. Our contact details are:
Telephone: 01642 624719
Freephone: 0800 092 0084
Opening hours: Monday to Friday, 9:30am to 4:00pm
Email: [email protected]
Out of hours
Out of hours if you wish to speak to a senior member of Trust staff, please contact the hospital switchboard who will bleep the appropriate person.
Telephone: 01642 617617
Patient, Public and People with Lived Experience
We are looking for patients to share their experiences of healthcare and to join our Involvement Bank. Working with the patients, carers, families and the general population we support in making decisions about their care can lead to better health outcomes, increased patient satisfaction and a better overall experience. We want to listen and work with you in shaping the future of your healthcare services. To find out more about the Involvement Bank go to our website or contact us at:
Website: www.nth.nhs.uk/about/community/people-with-lived-experience
Email: [email protected]
Data protection and use of patient information
The Trust has developed Data Protection policies in accordance with Data Protection Legislation (UK General Data Protection Regulations and Data Protection Act 2018) and the Freedom of Information Act 2000. All of our staff respect these policies and confidentiality is adhered to at all times. If you require further information on how we process your information please see our Privacy Notices.
Telephone: 01642 383551
Email: [email protected]
Privacy NoticesLeaflet feedback
This leaflet has been produced in partnership with patients and carers. All patient leaflets are regularly reviewed, and any suggestions you have as to how it may be improved are extremely valuable. Please write to the Clinical Governance team at:
Email: [email protected]
Leaflet reference: PIL1540
Date for Review: 14th August 2027