Information for patients
This leaflet can be made available in other formats including large print, CD and Braille and in languages other than English, upon request.
What is a distal radius fracture?
The radius is one of the two bones in the forearm, the other being the ulna. The distal part of the radius is the end nearest your wrist. This part of the radius is commonly broken. A small break at the end of the ulna often accompanies this injury.
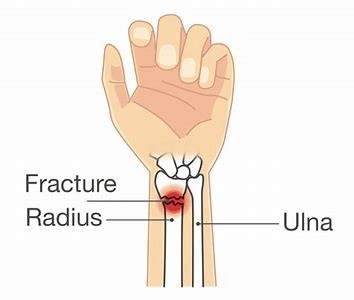
Distal radius fractures are very common. This fracture usually occurs as a result of a fall on to an outstretched hand.
Osteoporosis, a disorder in which bones become very fragile and more likely to break, can make a relatively minor fall result in a broken wrist. It mainly occurs in people older than 60 years of age. A broken wrist can happen even in healthy bones, if the force of impact is severe enough.
How do I manage distal radius fractures?
Depending on how bad the fracture is, surgical or non-surgical treatments may be chosen to achieve this goal. The goal of any treatment for this fracture is to hold the fracture in a satisfactory position to allow healing to occur.
Fractures are normally treated by holding with a splint or plaster cast for approximately four weeks, depending on the position and severity of the fracture.
If the bones have moved a lot out of position, you may need correction by surgery. Surgery may be required to fix the position of the bone and to insert metal fasteners (ORIF) to keep it in place. A cast will be applied following surgery and this will remain in place normally for two to six weeks.
Now that my plaster has been removed, what should I do next?
Once the Clinical Team have agreed it is safe for you to use and move your wrist, your cast will be removed. When the cast is first removed, it is normal to feel pain as your hand has not moved for some weeks, it may feel vulnerable too.
If you have been given a splint, wear this for the minimum recommended time, as wearing it for too long will restrict normal movement. Movement is important for the recovery process.
If you have been given pain relief, you should take them as prescribed. You should always read the label if using over-the-counter medication and, if you are in any doubt, speak to your pharmacist or GP. If your pain becomes severe or is continuous, you should contact your GP.
How should I care for my skin?
It is normal for your skin to feel dry and flaky when the cast is first removed.
Unless you have had an operation on your wrist, you should:
- Soak your hand and forearm in warm water, allowing your hand to float and move.
- Pat it dry with a towel and then moisturise thoroughly. Do this 2 to 3 times a day until the skin feels normal.
- Not pick or rub at the skin as this can make it sore.
If you have had a wound, do this as soon as the skin is fully healed, the scabs are off and the wound is dry.
What other advice can you provide me?
Swelling is a common problem post fracture. Raising your hand regularly throughout the day and completing hand exercises regularly help reduce this.
After your injury you may have been provided with a splint e.g. a Futura Splint. Initially, stop wearing the splint at home or when in low risk areas and then aim to stop wearing overnight and when in public spaces as well.
Begin to use your affected hand for light tasks (cutting food, drying up and getting dressed). Avoid heavy repetitive tasks in first 10 to 12 weeks. Avoid putting weight through your hand for 12 weeks after injury/surgery as directed by your therapist.
Following surgery for your wrist fracture, once your wound has healed and at least 48 hours after your stitches have been removed, you can start your scar massage. This will help increase blood circulation and promote a good quality scar. Scar massage is useful as it helps to breakdown the scar tissue. This allows the scar to move more freely and reduces the risk of the scar becoming sensitive.
Avoid swinging your arm down by your side (such as in brisk walking) for long periods of time, this will help to stop your hand from swelling.
Complex Regional Pain Syndrome (CRPS) is a poorly understood rare condition where a person experiences persistent severe and debilitating pain. Although most cases of CRPS are triggered by an injury, the resulting pain is much more severe and long-lasting than normal. The causes are largely unknown however it most commonly occurs following trauma.
It is very important to engage with early movement and sensory inputs as guided by your Physio to help minimise the risk of developing CRPS.
Factors such as:
- Stopping smoking,
- Controlling alcohol intake,
- Management of diabetes play a significant role in effective healing.
These factors, if not prevented or controlled, will increase inflammation in our bodies, which unfortunately reduces our ability to undergo effective healing. For further advice, please see useful links section.
The aim is for you to recover your range of movement and strength post injury. Evidence has shown that regular completion of exercises will improve your outcome post fracture.
What exercises can I do?
1) Tendon Glides


Keeping your knuckles straight, bend your fingers to make a hook first. Then from this position, roll your fingers into your palm to make a full fist. Return to the starting position.
Repetition: x10 Hold: 10 seconds Complete: Every 1 to 2 hours

Bend your knuckles, keeping the fingers straight. Then bend your middle knuckles so that your fingertips touch your palm. Return to the starting position.
Repetition: x10 Hold: 10 seconds Complete: Every 1 to 2 hours
2) Thumb Opposition

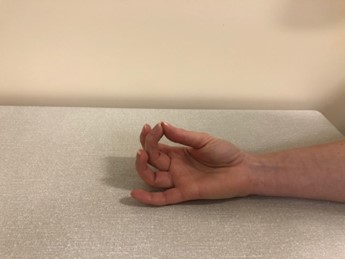



Place the back of your hand on a table. Use the tip of your thumb to touch the tip of each finger in turn. Once touching the tip of your little finger, slide the tip of your thumb down to the base of your little finger.
Repetition: x10 Hold: 5 seconds Complete: Every 1 to 2 hours
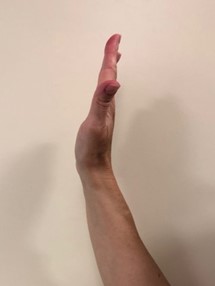
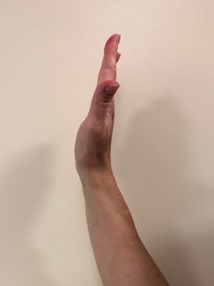
3) Wrist Extension Mobilisation

Sit with your forearm on a table and hand off the edge. Take your affected hand and lift it into an extension with your other unaffected hand.
Repetition: x10 Hold: 5 seconds Complete: Every 1 to 2 hours
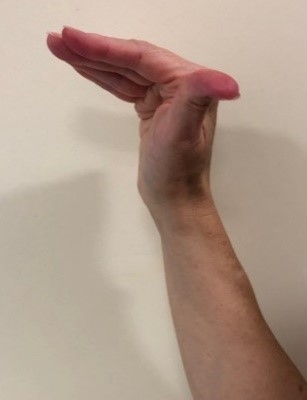
4) Wrist Flexion Mobilisation

Sit and rest your forearm on a table in front of you, letting your hand hang over the edge of the table. Bend your wrist towards the floor, helping yourself with the opposite hand.
Repetition: x10 Hold: 5 seconds Complete: Every 1 to 2 hours
5) Active Ulnar/Radial deviation



Put your wrist flat on a table with your forearm parallel to the floor. Use the opposite hand to stabilise your forearm just above your wrist. Move your wrist as much as you can from side to side, leaving it flat on the table at all times.
Repetition: x10 Hold: 5 seconds Complete: Every 1 to 2 hours
6) Active Pronation/Supination



Sit up straight in a chair with your forearm resting on a table.
With your elbow bent, turn your palm up to face the ceiling, then down to face the table, as much as possible turning only the forearm.
Repetition: x10 Hold: 5 seconds Complete: Every 1 to 2 hours
Useful Contacts
University Hospital of North Tees
Orthopaedic Outpatients
Telephone: 01642 624 486
University Hospital of Hartlepool
Orthopaedic Outpatients
Telephone: 01429 522 590
Physiotherapy Appointment Queries
Telephone: 01429 522 471
Monday to Friday, 09:00 a.m. to 04:30 p.m.
Other Useful Links
- Make Every Contact Count Gateway MECC – https://www.meccgateway.co.uk/nenc
- North Tees and Hartlepool NHS Foundation Trust Stop Smoking Service – https://www.nth.nhs.uk/services/stop-smoking-service/
- Advice and education on weight loss and maintain a healthy weight – https://www.nhs.uk/live-well/healthy-weight/
Comments, concerns, compliments or complaints
Patient Experience Team (PET)
We are continually trying to improve the services we provide. We want to know what we’re doing well or if there’s anything which we can improve, that’s why the Patient Experience Team (PET) is here to help. Our Team is here to try to resolve your concerns. The office is based at the University Hospital of North Tees if you wish to discuss concerns in person. Our contact details are:
Telephone: 01642 624719
Freephone: 0800 092 0084
Opening hours: Monday to Friday, 9:30am to 4:00pm
Email: [email protected]
Out of hours
Out of hours if you wish to speak to a senior member of Trust staff, please contact the hospital switchboard who will bleep the appropriate person.
Telephone: 01642 617617
Patient, Public and People with Lived Experience
We are looking for patients to share their experiences of healthcare and to join our Involvement Bank. Working with the patients, carers, families and the general population we support in making decisions about their care can lead to better health outcomes, increased patient satisfaction and a better overall experience. We want to listen and work with you in shaping the future of your healthcare services. To find out more about the Involvement Bank go to our website or contact us at:
Website: www.nth.nhs.uk/about/community/people-with-lived-experience
Email: [email protected]
Data protection and use of patient information
The Trust has developed Data Protection policies in accordance with Data Protection Legislation (UK General Data Protection Regulations and Data Protection Act 2018) and the Freedom of Information Act 2000. All of our staff respect these policies and confidentiality is adhered to at all times. If you require further information on how we process your information please see our Privacy Notices.
Telephone: 01642 383551
Email: [email protected]
Privacy NoticesLeaflet feedback
This leaflet has been produced in partnership with patients and carers. All patient leaflets are regularly reviewed, and any suggestions you have as to how it may be improved are extremely valuable. Please write to the Clinical Governance team at:
Email: [email protected]
Leaflet reference: PIL1525
Date for Review: January 2028