Information for patients
This leaflet can be made available in other formats including large print, CD and Braille and in languages other than English, upon request.
This leaflet gives dietary advice for after your ESG and has been developed by Bariatric (weight loss) Dietitians. If you have any questions or concerns, please contact the Bariatric Nurse Specialists and Dietetics department (details at the end of this leaflet).
Food reintroduction after ESG
After your procedure you will need to go through several stages of food reintroduction, slowly progressing from liquids through to solid food. This is to give the stitches time to heal well.
If you do not follow the dietary recommendations, there is a risk of loosening the stitches.
Stage 1: Liquid diet (weeks 1 to 6)
- Start with sips and, if these feel comfortable, gradually increase the amount you take in one go.
- It is fine to drink (for example, tea, coffee, squash, water), but you should make sure these are in addition to high protein liquids and not instead of them.
High protein liquids
- Milk with added milk powder (make at home by mixing 1 pint of semi-skimmed or skimmed milk with 4 tablespoons of dried skimmed milk powder).
- Smoothies (fruit or vegetables blended with milk with added milk powder, high protein yoghurt or protein powder). Homemade will be better as shop-bought varieties may be high in sugar.
- Smooth soup (homemade or tinned) with an added 1 to 2 tablespoons of skimmed milk powder or unflavoured protein powders. Avoid instant cup-a-soups.
- Meritene® shakes and soups (available in pharmacies).
- Complan® shakes and soups (available in supermarkets and pharmacies).
- Meal replacement shakes (such as Slimfast® (powders or ready to drink – available in supermarkets), Tesco Slim® or Asda Great Shape®, Exante® or Lighter Life® (available online).
- High protein milkshakes (such as, Ufit®, Arla®, For Goodness Shakes®, Urban Active®).
- Protein water (such as Vievé®, Upbeat® or +PW®).
- Whey, soya or pea protein powders, made into a shake as in instructions (available in health food shops and some pharmacies).
Stage 2: Soft diet (weeks 7 and 8)
Food at this stage should be soft enough that it will fall apart when pressed with a fork or spoon. You should eat 3 small, soft meals a day and avoid grazing throughout the day.
Listen to your body and when you feel satisfied, stop.
You should aim to balance your meals according to the small dinner plate below, with half of your meal being protein, a quarter vegetables or fruit and a quarter carbohydrate.
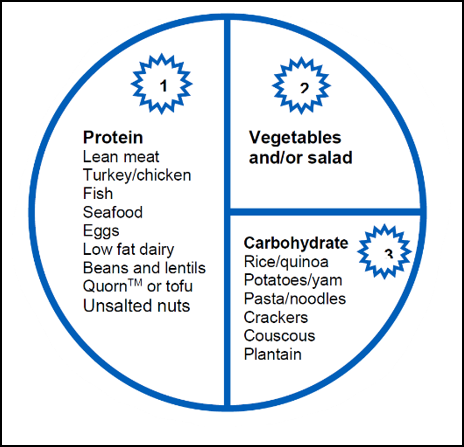
Choose a high protein option and add small amounts of soft vegetables and carbohydrate – see examples next in this leaflet.
Example meal plan
Choose one from each group
Breakfast
- Low fat, high protein yoghurt with soft fruit.
- Weetabix® or other cereal softened with milk with added milk powder.
- Porridge or Ready Brek®.
- Soft cooked egg (poached, scrambled) with a tinned tomato.
- Homemade fruit smoothie (fruit blended with yoghurt or milk).
- Protein or meal replacement shake.
Main meals
Two a day – lunch and evening meal
- Crackers or crispbreads with high protein topping (tinned fish, cottage cheese, mashed egg, low fat soft cheese, hummus).
- Omelette (1 to 2 eggs) with cheese.
- Lasagne, Ravioli or Spaghetti Bolognese (soft pasta dishes).
- Shepherd’s or Cottage pie.
- Fish in sauce or fish pie with soft cooked vegetables.
- Tuna pasta bake (with soft cooked pasta).
- Meat/chicken stew with vegetables and boiled/mashed potato/cassava/plantain.
- Mince in gravy with vegetables and boiled/mashed potato.
- Baked beans with boiled/mashed potato.
- Chunky, high protein soup (such as, minestrone, pea and ham, Tuscan bean).
- Lentil dhal.
- Meat/chicken and vegetable curry (avoid rice or bread for now).
Stage 3: Regular diet (week 9 onwards)
You are now ready to continue on your long-term eating plan. Remember that you are not just eating small amounts to reduce your calorie intake and lose weight.
You should also be aiming for a healthy nutritious eating plan.
- Eat three meals each day. Avoid skipping meals, even if you don’t feel hungry, as going for long periods without eating can actually slow down weight loss.
- Eat slowly and stop as soon as you feel full. Rushing your meals can lead to overeating as there is a delay between eating and your brain realising that you are full. Eating too quickly often means you won’t be chewing your food properly.
- Protein, vegetables, carbohydrates. This is the order in which you should eat from your plate. Protein is the most important part, so eat that first in case you become full before you clear the whole plate. Carbohydrates are least important, so eat those last and don’t worry if you cannot finish them.
- Eat a healthy, balanced, solid diet. Choose solid foods (such as lean meat or fish with vegetables) as these stay in the stomach for longer and are more satisfying. You will eat less overall and stay fuller for longer. Follow a diet, based on healthy eating guidelines, that is low in fat and sugar and high in lean protein and fibre.
- Small portions. Your meals should be no larger than the size of a ‘side plate’ or ‘tea plate’. We suggest that you switch to using one of these plates long-term to help you control your portions.
- Be cautious of unplanned snacking. Try not to develop a ‘grazing’ pattern of eating small meals throughout the day.
- Choose low calorie drinks (non-carbonated). Liquids pass through your stomach quickly and easily, and high-calorie drinks will add calories to your daily intake without filling you up. High-calorie drinks include alcohol, fruit juices, smoothies, sweetened (sugar-containing) squash/cordial, non-diet soft drinks, sports drinks, milk and milk-based drinks such as milkshakes. Milk is a good source of calcium and low-fat milk in reasonable quantities is fine, but other high-calorie liquids should be limited. Avoid all fizzy drinks as these can create pressure in the stomach and cause discomfort and possibly lead to the stomach stretching.
For best weight loss, limit the following foods:
- High calorie drinks (alcoholic drinks, fruit juice or smoothies, full-fat milk or milky drinks such as hot chocolates, milky coffees or milkshakes, sugar-sweetened soft drinks, energy drinks).
- Chocolate, ice-cream, cakes, sweets, biscuits and desserts rich in sugar or fat.
- Added fats and fatty foods – butter, oils, cream, full fat dairy, fried foods, fatty meats.
- High fat savoury snacks foods such as crisps, pastries and nuts.
Cooking tips
- Remove all fat and skin from any meat or chicken before cooking.
- Use low fat cooking methods such as grilling, baking (wrap in foil to keep things moist), steaming or boiling.
- Limit oil or butter added to vegetables or salads. If you need extra flavour, add seasoning or a little bit of low-calorie dressing or vinegar.
- If you need to use oil to stop food from sticking, use a spray oil.
- Add flavour using herbs, spices, seasonings, lemon juice, ginger, onions, and garlic.
- Do not add any oil or butter to carbohydrates – keep them simple.
- Choose high fibre carbohydrate options wherever possible as these will keep you fuller for longer and help to prevent constipation (try wholegrain bread, pasta, rice, crackers and keep skins on potato).
Multivitamins and minerals after ESG
After your procedure, it is unlikely that you will be able to get all the vitamins and minerals essential for good health from your food alone so it is important that you take a multivitamin and mineral supplement:
Please purchase a multivitamin and mineral supplement, such as
- Aldi everyday health (Twice daily) OR
- Asda A – Z (Twice daily) OR
- Sanatogen A – Z (Twice daily) OR
- Tesco A – Z (Twice daily)
Your GP will prescribe:
- Vitamin B12 Injections 3 months post op and to continue this regime every 3 months lifelong, no loading dose required.
- lansoprazole 60mgs daily for 2-year post op
- Calcium carbonate with colecalciferol — ADCAL -D3— 1.5g + 400 units chewable tablet (DOSE 1 tablet(s) — Oral — With Lunch and Evening Meal — Lifelong)
Long-term nutritional monitoring
It is also important that you have regular blood tests to monitor for nutritional deficiencies (you not having enough of a vitamin or mineral in your body). You should have bloods at 6 and 12 months in the first year and annually thereafter.
Contact Numbers
If you need further advice or have any problems, please contact the appropriate number below:
North Tees and Hartlepool NHS Foundation Trust
Bariatric Nurse Specialist
Telephone: 01642 624601
Monday to Friday, 9.00am to 5.00pm
Dietitian
Telephone: 01429 522471
Monday to Friday, 9.00am to 5.00pm
Consultant’s secretary
Telephone: 01642 383292 or 01642 383290
Monday to Friday, 9.00am to 5.00pm
Further information is available from:
The NHS website at www.nhs.uk
Leaflet reproduced with kind permission from Professor Bu’Hussain Hayee at King’s College Hospital.
Comments, concerns, compliments or complaints
Patient Experience Team (PET)
We are continually trying to improve the services we provide. We want to know what we’re doing well or if there’s anything which we can improve, that’s why the Patient Experience Team (PET) is here to help. Our Team is here to try to resolve your concerns. The office is based at the University Hospital of North Tees if you wish to discuss concerns in person. Our contact details are:
Telephone: 01642 624719
Freephone: 0800 092 0084
Opening hours: Monday to Friday, 9:30am to 4:00pm
Email: [email protected]
Out of hours
Out of hours if you wish to speak to a senior member of Trust staff, please contact the hospital switchboard who will bleep the appropriate person.
Telephone: 01642 617617
Patient, Public and People with Lived Experience
We are looking for patients to share their experiences of healthcare and to join our Involvement Bank. Working with the patients, carers, families and the general population we support in making decisions about their care can lead to better health outcomes, increased patient satisfaction and a better overall experience. We want to listen and work with you in shaping the future of your healthcare services. To find out more about the Involvement Bank go to our website or contact us at:
Website: www.nth.nhs.uk/about/community/people-with-lived-experience
Email: [email protected]
Data protection and use of patient information
The Trust has developed Data Protection policies in accordance with Data Protection Legislation (UK General Data Protection Regulations and Data Protection Act 2018) and the Freedom of Information Act 2000. All of our staff respect these policies and confidentiality is adhered to at all times. If you require further information on how we process your information please see our Privacy Notices.
Telephone: 01642 383551
Email: [email protected]
Privacy NoticesLeaflet feedback
This leaflet has been produced in partnership with patients and carers. All patient leaflets are regularly reviewed, and any suggestions you have as to how it may be improved are extremely valuable. Please write to the Clinical Governance team at:
Email: [email protected]
Leaflet reference: PIL1543 version 2
Date for Review: February 2028