Information for patients
This leaflet can be made available in other formats including large print, CD and Braille and in languages other than English, upon request.
What is Chronic Pelvic Pain (CPP)?
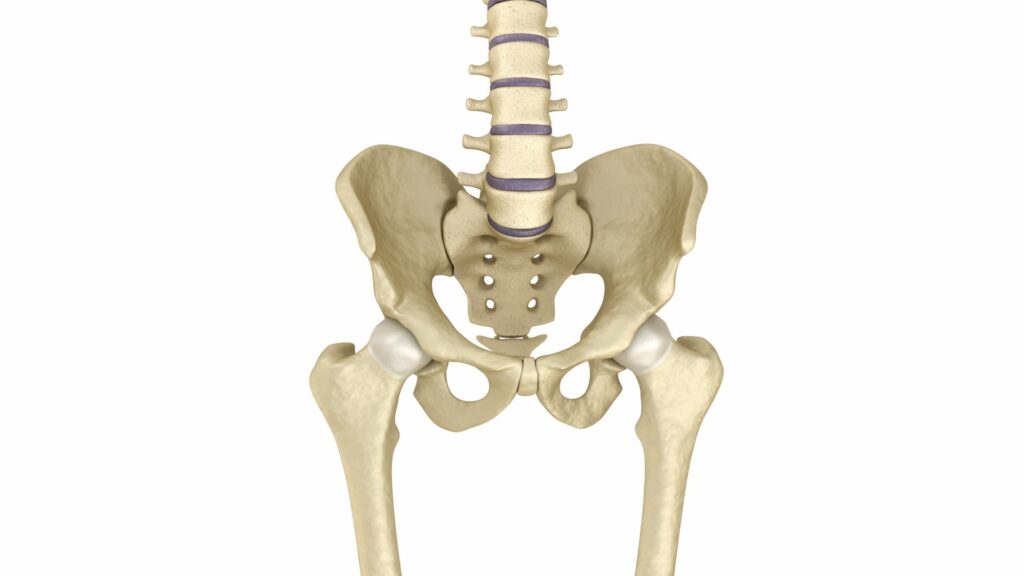
Your pelvis is between is the lower part of your tummy and your legs. Please see the diagram below.
Any pain that lasts longer than 6 months in this region is called Chronic Pelvic Pain (CPP). This condition can affect 1 in 6 women. CPP can cause a lot disruption to someone’s life and can be very distressing. This is why we have created this leaflet to try to help you understand the condition and to explain available treatments.
What causes CPP?
There are many possible causes of pelvic pain. CPP can be a combination of physical, psychological and social problems.
The condition is sometimes not fully understood by people who do not have it, and the pain experienced can be different for each person due to a number of different reasons.
Organs in your pelvis include your bowel (part of your digestive system), bladder, womb (uterus), ovaries and your fallopian tubes. Pelvic pain usually starts from one of these organs.
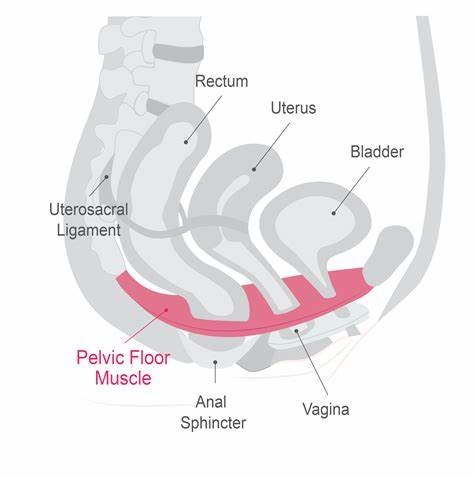
In some cases, the pain comes from your pelvic bones that are next to these organs, or from nearby muscles, nerves, blood vessels or joints.
There are a number of physical problems that can cause CPP. These include:
- Endometriosis – This is a condition where the cells of the lining of the womb (endometrium) are found elsewhere in the body, usually the pelvis.
- Adenomyosis – A condition where the lining of the womb (endometrium) is found in the muscle of the womb which can cause pain around the time of a period and during sex.
- Pelvic inflammatory disease – This is an infection in the fallopian tubes and/or pelvis.
- Interstitial cystitis – Bladder inflammation.
- Adhesions – Areas of scarred tissue that may be a result of a previous infection, endometriosis or surgery.
- Trapped or damaged nerves in the pelvic area.
- Pelvic organs prolapse.
- Musculoskeletal pain – Pain in the joints, muscles, ligaments, and bones of the pelvis.
- Irritable Bowel Syndrome (IBS).
Neuropathic Pain
Sometimes, there may never be a physical condition linked to your pain.
In these cases, the problem could be in the perception of pain by nerve endings in the pelvis. The pain can still be felt after the physical damage has healed. Long lasting pain can cause changes in how your brain understand pain.
You can have damage to your nerves from an infection, from surgery or trauma (injury), or from fibrosis (excess tissue from scarring).¹
Patients who have this damage and are more sensitive to pain can find that the pain is triggered very easily. This can be very distressing for people.
Psychosocial causes
An unstable mental health can also cause an increase in the sensitivity of pain.
There is a chance that CPP could lead to further mental health problems. This could cause a vicious cycle where each condition makes the other worse, reducing your quality of life significantly.
What will my Doctor do?
Your Doctor will take a detailed history from you about your pain pattern. This will help to work out if it is related to your periods or sex, or if pain is constant.
Any information about previous surgeries, sexually transmitted infections, bowel or bladder issues which contribute to the pain will be discussed.
Your Doctor will also ask you about any musculoskeletal problems such as backache or joint problems that you may be aware of.
Any psychological factors such as depression, anxiety and abusive relationships will also be discussed.
If you are suffering from depression or anxiety, these factors still may not be the cause of your CPP. Your Doctor will discuss this further with you.
It is well known that stress, anxiety and depression release chemicals that exaggerate pain sensitivity.4 If this is the case, treatment should be directed to treat any psychological issues. This can lead to endorphins (hormones that make you feel happy) being released, which will lead to physical pain being eased.
What will happen during my exampination?
Your Doctor will ask you to have a physical examination. This includes an internal examination of your vagina. Your examination is essential to work out what is causing your pain, and to locate the precise pain-sensitive area. You will be given a choice to proceed with examination, and who undertakes this, where possible. A chaperone will also be in the room throughout the examination.
If the examination is too painful, can ask the doctor to stop. You are free to tell the doctor to stop at any time. Any internal examination will only take place if you are comfortable for this to happen.
What tests will be requested?
- Screening tests for sexually transmitted infections – Screening tests for sexually transmitted infections are vaginal swabs to rule out infection, these will only be obtained with your consent.
- Urine test – A urine test is completed on initial appointment in order to rule out any underlying infection which could be impacting your chronic pelvic pain.
- Ultrasound or an MRI – An Ultrasound or MRI scan are investigations that can provide further insight for the clinician in order to make further decisions. These are not always required and will be discussed with you in clinic prior to being requested.
- Laparoscopy – Laparoscopy is commonly known as keyhole surgery. It involves general anaesthesia, 3 to 4 small cuts in your tummy and your Doctor looking at your pelvis using a small telescope.
This may help find a physical disease, which can usually be treated at the same time. If the disease is extensive, you may be offered a repeat surgery.
There is a 1 in 4 chance that your laparoscopy is not able to determine the cause of your pain. While this can be reassuring for some women, it may also lead to frustration for others.
Your Doctor will discuss ways to deal with the pain after further examination of your symptoms and history.
How will I be treated?
At first, you will be offered pain relief. Any other treatments will depend on your symptoms and diagnosis.
- If a diagnosis of endometriosis/adenomyosis is made, you may be offered hormones. This will either be in the form of pills, injections or a coil.
2. If you have suffered from an infection, your Doctor will prescribe you with antibiotics.
3. Your Doctor may recommend keyhole surgery if other treatments have not worked.
If your symptoms suggest bowel, bladder or musculoskeletal problems, you will be referred to the appropriate department.
If no physical disorder is found, either your Doctor or the pain team that you are referred to may prescribe you some medication. This may include drugs that are traditionally used to treat epilepsy or depression. This medicine will change the way your nerves and brain process pain. These are called pain modifiers.3
Current research suggests that complementary therapies, such as psychological counselling, acupuncture, mindfulness exercises and diet changes may help improve your symptoms. Your Doctor may recommend one of these therapies or refer you to a specialist who offer one of these therapies.2
Many women find that they can cope better with the pain if they have been listened to, taken seriously, have a full explanation of their test results and agree a plan of action. You may be reassured by finding that nothing is seriously wrong and the pain may get better with time.
Chronic pelvic pain can be very difficult to live with and can cause emotional, social and economic difficulties. You may experience depression, difficulty sleeping and disruption to your daily routine. Talk to your GP if this is the case.
The support of other women who also experience pelvic pain may also help. See below for information about support groups.
Further information and support groups
- IBS Network: www.theibsnetwork.org
- Pelvic Pain Support Network: www.pelvicpain.org.uk
- Bladder & Bowel Foundation: www.bladderandbowelfoundation.org
References
- Patient Info: Pelvic Pain in Women; Author: Dr. Doug McKenchnie, MRCGP, Updated by: Dr. Hayley Willacy. Pelvic Pain in Women: Causes, Symptoms, and Treatment https://patient.info/womens-health/pelvic-pain-in-women [Last Accessed: 13/05/2025]
- The University of Edinburgh 2021. Pain where no cause is found during investigations available at: https://www.ed.ac.uk/centre-reproductive-health/exppect-pelvic-pain/information-for-patients/conditions/pain-no-cause-found [Last Accessed 13/05/2025].
- Royal College of Obstetricians and Gynaecologists. Long-term Pelvic Pain. London: RCOG; 2015 https://www.rcog.org.uk/for-the-public/browse-our-patient-information/long-term-pelvic-pain/[Last Accessed 14/04/2025].
- The University of Edinburgh. 2021. Persistent pelvic pain. available at:https://www.ed.ac.uk/centre-reproductive-health/exppect-pelvic-pain/information-for-patients/persistent-pelvic-pain [Last Accessed: 13/05/2025].
Comments, concerns, compliments or complaints
Patient Experience Team (PET)
We are continually trying to improve the services we provide. We want to know what we’re doing well or if there’s anything which we can improve, that’s why the Patient Experience Team (PET) is here to help. Our Patient Experience Team is here to try to resolve your concerns as quickly as possible. The office is based on the ground floor at the University Hospital of North Tees if you wish to discuss concerns in person. If you would like to contact or request a copy of our PET leaflet, please contact:
Telephone: 01642 624719
Freephone: 0800 092 0084
Opening hours: Monday to Friday, 9:30am to 4:00pm
Email: [email protected]
Out of hours
Out of hours if you wish to speak to a senior member of Trust staff, please contact the hospital switchboard who will bleep the appropriate person.
Telephone: 01642 617617
Data protection and use of patient information
The Trust has developed Data Protection policies in accordance with Data Protection Legislation (UK General Data Protection Regulations and Data Protection Act 2018) and the Freedom of Information Act 2000. All of our staff respect these policies and confidentiality is adhered to at all times. If you require further information on how we process your information please see our Privacy Notices.
Telephone: 01642 383551
Email: [email protected]
Privacy NoticesLeaflet feedback
This leaflet has been produced in partnership with patients and carers. All patient leaflets are regularly reviewed, and any suggestions you have as to how it may be improved are extremely valuable. Please write to the Clinical Governance team, North Tees and Hartlepool NHS Foundation Trust, University Hospital of North Tees, TS19 8PE or:
Email: [email protected]
Leaflet Reference: PIL1366 – Version 02
Date for Review: 04/06/2028