Information for patients
This leaflet can be made available in other formats including large print, CD and Braille and in languages other than English, upon request.
This leaflet tells you about Cholecystectomy procedures.
What is Cholecystectomy?
A Cholecystectomy is an operation to remove your gallbladder.
This operation can be done laparoscopically or as an open procedure.
Laparoscopic – The operation is carried out with a laparoscope (viewing instrument), which is inserted into your abdomen (tummy). This is also known as keyhole surgery. This means your recovery will be quicker.
Open – The operation is carried out as an open procedure through an incision (cut) in your abdomen.
Your operation will be performed under a general anaesthetic (a state of carefully controlled and supervised unconsciousness (deep sleep) that means you are unable to feel any pain).
One of your doctors will explain to you the type of procedure you will be having and the reason for your operation. They will further explain the operation itself and precautions they will take to avoid any risks and complications.
What does the gallbladder do?
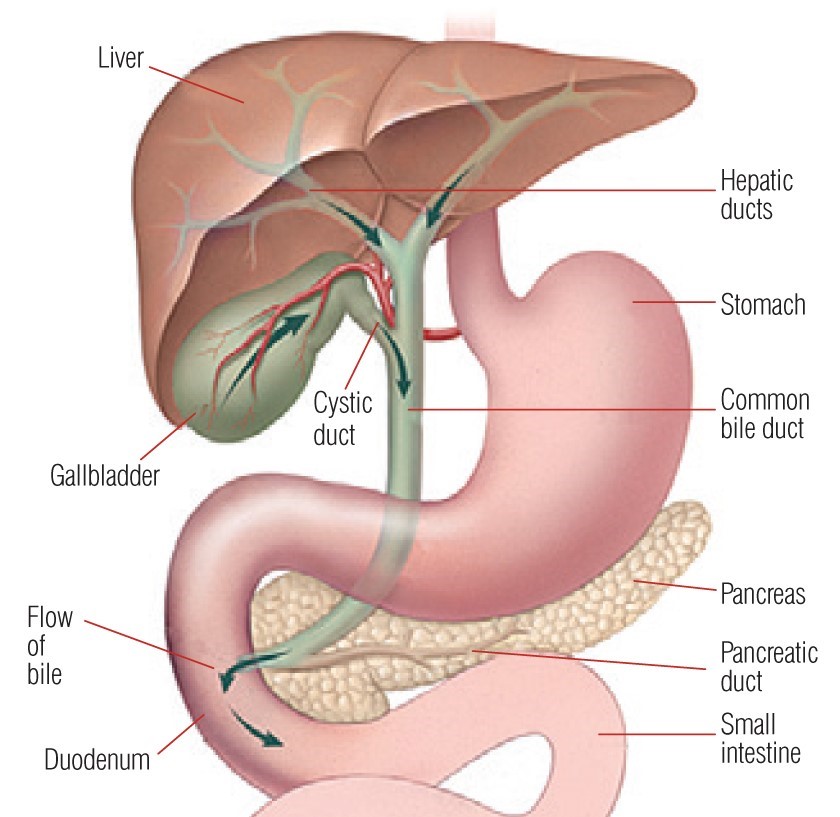
The Gallbladder is a small, pouch like organ, which sits underneath the liver. Its function is to store and concentrate bile, the liquid which helps to break down fats in our diet. It is released after eating a meal and drains into the duodenum through the common bile duct. Stones can be formed in the Gallbladder and also in the common bile duct.
(See diagram on next page)
Why do some people develop gallstones?
It is not known why some people develop gallbladder disease.
There are several factors which can make people more likely to develop gallstones and these include:
- Heredity – Gallstones tend to run in families.
- Gender – Women are twice as likely as men to have gallstones.
- Pregnancy – Pregnancy causes oestrogen (female hormone) levels to rise that can increase the risk of gallstones developing.
- Body weight -Being overweight increases the amount of cholesterol in your bile. This extra cholesterol may form into crystals and eventually into gallstones.
- Lifestyle -Diets high in fat and sugar, low calorie diets and rapid weight loss can disrupt the bile chemistry and make it more likely for gallstones to develop.
- Age – The chance of developing gallstones increases with age.
- Previous bowel surgery -Some operations to the bowel can increase the risk of developing gallstones.
- Common bile duct stones – Stones can slip from the gallbladder and into the bile duct.
Are there any risks or complications of having a Cholecystectomy and Common Bile Duct Exploration?
As with any surgical procedure, a cholecystectomy has some risks. These can vary according to your age and other illnesses you may have. The risks can include:
- Pain. This could be shoulder tip or abdominal pain due to irritation from the air used in your abdomen so your surgeon can see your organs.
- Bleeding. You may develop bleeding inside your abdomen or from your wounds after your operation. If this occurs, it will be treated as needed. You may need a blood transfusion or another operation, in extreme circumstances.
- Wound infection. After you have been discharged, if you feel feverish and your wound becomes hot, red and sticky, you should see your GP. This can be treated with antibiotics, and you will not usually need to be re-admitted to hospital.
- Scarring. You will have very small scars following surgery from the incision sites if you have had a laparoscopic procedure or a slightly larger scar if you had an open procedure.
- Haematoma/collection. A collection of blood can sometimes develop at the wound site or inside the abdomen. This may require drainage or returning to theatre.
- Bile leak. The bile can leak from your cystic duct or from the bile duct and also from the liver surface where the gallbladder is attached. Less than 3 out of 200 patients experience a bile leak after gallbladder surgery. If this happens, in many cases, this will settle down in a few weeks or you may need a drain inserting. You might go home with a drain, or you might need a further procedure to stop this. Your doctor will discuss with you and explain further.
- Bile duct injury. Approximately 3 – 4 people in every 100 will suffer injury to the bile duct during surgery. If this happens, you may require another operation or procedure. ¹
- Bile Duct Narrowing (Stricture) – There is a small possibility in the long term that bile duct stricture can occur after bile duct exploration.
- Change to open surgery. If you are having a laparoscopic operation, your surgeon may need to convert to an open procedure. The reasons this may be needed include the presence of adhesions (scar tissue) from previous surgery, bleeding and accidental injury to internal organs. Approximately 1 in 20 people require a conversion from keyhole surgery to an open procedure.
- Injury to surrounding structures. These can include bowel, liver and blood vessels. If this happens, these will be repaired at the time of your operation.
- Dropped/slipped gallstones. This is when the gallbladder stones fall into the abdominal cavity and remain there during surgery. This happens to 16 out of every 100 people having this procedure.² This can cause an abscess to develop and may need further treatment. Sometimes gallstones can also slip into the bile duct after surgery, which may require you to have a further procedure.
- Missed common bile duct stone. There is a small possibility of missing common bile duct stone while assessing the bile duct with intraoperative ultrasound.
- Retained stones. If you undergo bile duct exploration as treatment for your common bile duct stones, there is a possibility of a stone being left behind. Your surgeon will discuss this during the consent process.
- Deep vein thrombosis – DVT (blood clots in the leg veins) or pulmonary embolism – PE (blood clots in the lungs). Sometimes a clot forms in the deep veins of the leg after an operation. This can cause your leg to swell and become painful. If the blood clot in the vein becomes dislodged, (moves) it can travel to the lung and cause a PE.
A DVT or PE can be due to the effects of the surgery or reduced activity during . your recovery.
All adult patients will have their risk of developing a blood clot assessed within 12 . hours of admission. Patients who are being admitted for planned surgery may have . their risk assessed at pre-assessment.
The nurse or doctor who carries out your assessment will discuss your risk factors with . you and advise on treatment to reduce your risk.
- Risks associated with a general anaesthetic. Your anaesthetist (a doctor with special training in anaesthetics) will discuss this with you.
- Post-cholecystectomy syndrome/Non-Resolution of Symptoms. You may suffer from symptoms of tummy pain, acid reflux (heartburn), diarrhoea or jaundice (yellowing of the eyes and skin) following removal of your gallbladder. If you develop any of these symptoms, you may need further tests to evaluate the situation and depending on the results, you might require further treatment.
- Diarrhoea. Very occasionally chronic diarrhoea may develop following a Cholecystectomy. Medication may be required to treat this.
- Port site hernia (when an internal part of the body pushes through a weakness in the muscle or surrounding tissue at the site of surgery). Some patients can develop a hernia where the cuts to the abdomen were made during laparoscopic procedure.
What will happen at the pre-assessment clinic?
You will meet the nurse practitioner who will explain your operation and answer any questions you may have. The nurse will complete your admission forms and start to discuss and plan your discharge from hospital after your operation.
Some routine health checks will be taken at the clinic, for example, blood and urine tests, ECG (heart tracing), and X-rays if required. You can expect your appointment to last between 1 to 3 hours depending on what tests and checks need to be done. If you are admitted as an emergency, the anaesthetist will assess you at the time of your surgery.
Why am I asked not to eat or drink before my operation?
Your nurse will tell you when you must stop eating or drinking before your operation. This is very important. You must follow the instructions. Nothing means nothing at all, including water and chewing gum.
If you forget and do eat or drink anything you must tell your doctor or nurse, as your operation may need to be postponed for your safety. This is because when you are unconscious, if your stomach contains food or drink you may be sick and it could get into your lungs, affect your breathing and cause an infection.
What do I need to bring with me?
The National Institute for Health and Care Excellence (NICE) recommends that you keep warm, before, during and after your operation because it can reduce side effects, complications and help you recover from your operation faster.¹
Please make sure you bring socks and slippers, a dressing gown, a vest or other warm clothing to help you feel warm while you are in hospital. Please arrange for someone to collect your clothing and any items you will not need while you are in hospital, as storage space on the wards is limited.
Please bring in all medicines that you are taking. If doses of any other medicines change after your pre-assessment visit, you must tell your nurse or doctor when you are admitted.
How can I prepare for my operation?
Before any operation it helps to try and get as fit as possible as this helps in your recovery.
The most common types of gallstones are made of cholesterol and can be managed by changing your eating habits; by reducing the amount of fatty foods you eat and keeping your weight down.
If you are overweight, seek advice from your GP or practice nurse who will offer you support and dietary advice. Losing weight will help to reduce risks or complications during your operation.
If you smoke, it is advisable that you stop. Smokers are more likely to develop chest infections or blood clots after surgery. We realise this can be difficult, but your GP, practice nurse and staff on the ward are able to offer you advice and support.
What will happen before my operation?
When you arrive, one of the nurses who will care for you will welcome you to the Access Lounge. They will re-check your details taken at the pre-assessment clinic to make sure nothing has changed.
One of your doctors will see you shortly after your arrival. They will tell you the planned time of your operation and answer any questions you may have.
Before the operation, one of the doctors will again explain the reasons for the operation, the operation itself and the precautions we take to avoid any risks or complications. When you fully understand the operation and you are happy to proceed, you will be asked to sign a consent form.
You will be asked to remove any jewellery you are wearing (except your wedding ring), contact lenses, make-up and nail varnish and you are asked not to use any body lotions, deodorants and perfumes. You will be asked to put on a theatre gown and you will be fitted with surgical stockings to help prevent blood clots (DVT).
False teeth, glasses and hearing aids may be removed in the operating theatre.
You may be given a ‘pre-med’ (some tablets to help you relax).
Just before the time of your operation, one of your nurses will go with you and transfer your care to a theatre nurse.
If you have any worries or concerns tell the staff, they are there to help and support you.
Your theatre nurse will check your details again before taking you into the anaesthetic room. In the anaesthetic room, you will meet your anaesthetist again. They will give you an anaesthetic before you are taken to the operating theatre.
If your temperature is below 36°C (98.6°F), the operation will not start until you are warm. A warm air blanket or jacket may be used to raise your temperature.
When in the operating theatre and the recovery room, your nurse will take your temperature regularly. If it falls below 36°C (96.8°F), you will be placed under a warm air blanket or jacket.
Please tell your nurse if you feel cold during your stay in hospital.
Before and during your operation:
- A cannula (fine needle) will be placed in the back of your hand or arm so we can give you medication. Sometimes, when drugs are injected they may feel cold and sting a little.
- An intravenous drip may be attached to your cannula, but this usually takes place when you are asleep.
- You may be asked to breathe oxygen through a facemask before you are given the anaesthetic.
- Your blood pressure will be taken.
- Your pulse will be taken and the amount of oxygen in your blood will be measured by attaching a special clip to your finger. This does not hurt.
- Your heart rate will be monitored by placing sticky pads on your chest. These are attached to some leads to show a tracing of your heart on a monitor. This is routine and is nothing to worry about.
What will happen while I am in hospital?
On admission to the ward, you will be introduced to your ‘named
nurse’ who is responsible for planning your nursing care with you. Your ‘named nurse’ is part of a team of nurses who are there to help and advise you and to make your stay as comfortable as possible.
What will happen during my operation?
Laparoscopy
You will have small incisions in your abdomen. Your abdomen will be filled with air so that the laparoscope can be inserted safely, and the organs can be seen clearly.
The laparoscope allows the surgeon to see the inside of your abdomen. It is also possible to pass instruments through the small cuts in your abdomen to remove your gallbladder.
Intra-operative ultrasound and common bile duct exploration
At that time of your gallbladder surgery your surgeon, with the help of a flexible instrument (Laparoscopic ultrasound) will assess the bile duct to look for any stones in it. If any stones are found in the common bile duct and if the duct is big enough, the surgeon will proceed to remove the stones at the same time. A small cut is made in the bile duct and a camera is passed up and down the duct to visualise (see) the stones before removing them. The opening in the duct is then closed using sutures. If you have stones and the duct is small, you will need a camera test (ERCP) after the gallbladder operation to remove the stone in the bile duct. When the surgeon is finished, the air is released.
If the cystic duct is big enough, the surgeon will be able to pass the instrument to remove the stones in the bile duct, without need to open the bile duct. All these things will be discussed with you and explain in detail during the consent process.
The small wounds are closed either by using dissolvable sutures (stitches) or by sutures which need to be removed by the practice nurses at your GP’s practice. Your nurse will tell you which type you have.
Open
An incision will be made in your upper abdomen. Your gallbladder will be removed, and the wound will be closed using either dissolvable sutures (stitches) or clips which will need to be removed by the practice nurses at your GP practice. Your nurse will tell you which type you have.
What will happen after my operation?
- After your operation, you will be taken to the recovery room. Not everyone remembers waking up in the recovery room. Specially trained nursing staff will look after you until you are ready to return to your ward.
- If you have any pain or feel sick, let the nursing staff in the recovery room know. They will give you some medication to relieve it, so by the time you are transferred back to the ward you should feel comfortable.
What will happen once I am back on the ward after my operation?
- When you are taken to the ward, you will be made comfortable. Your nurse will check your blood pressure, pulse, temperature, pain level and wound. You will be encouraged to sit up and move around to prevent complications such as chest infections and Deep Vein Thrombosis (DVT).
- We may give you pumping devices on your legs to help prevent blood clots.
- If at any time you are in pain or feel sick, please let one of your nurses know and they will give you medication to relieve it.
- Your nurse will tell you when you can start to drink again, usually a few hours after your operation. You will have an intravenous drip in your arm through which you will receive fluids to prevent you from becoming dehydrated until you are able to drink normally.
- Your wounds will have dressings over them, which will allow you to bathe or shower from the day after your operation.
- You may have a drain in your abdomen. This is a very thin tube which sits underneath your skin and drains away any fluid or bile that might collect inside the abdomen. The surgeon will explain and discuss with you when the drain will be removed.
- Sometimes, if you have common bile duct exploration your surgeon may place a plastic stent or a T-Tube inside your bile duct if they think it is necessary at the time of procedure. The surgeon will discuss this at the time of consenting.
- The small hole from the drain site that remains will close up on its own. Sometimes it may ooze fluid for a little while. If needed, a dressing will be put over it. You will be able to bathe or shower with the dressings.
You may have:
- Some discomfort in your upper abdomen and shoulders. This is due to the air, which was pumped into your abdomen and should get better in 2 – 3 days.
- Colic-like (cramping) abdominal pain for a few days after your laparoscopy. It is important to walk around to help get rid of the air.
- Discomfort from your wound sites. Taking painkillers at regular intervals works best, rather than waiting until you are in pain. It will also reduce the need to take stronger painkillers. Always follow the instructions provided in the leaflet supplied with your tablets.
- Some nausea (feeling sick) or vomiting (being sick) due to the effects of the anaesthetic. These will usually settle within 24 – 48 hours. It is important to drink plenty of fluids but not alcohol, to avoid dehydration.
It is normal to feel tired for 24 to 48 hours after your operation. A little bruising may develop around your wound sites, but this will clear.
Will I be in pain after my operation?
After all operations some discomfort, soreness or pain is to be expected, so good pain relief is important. It helps you feel better and makes it easier for you to move around, take deep breaths and cough. This reduces the risk of any complications happening after surgery.
- Painkiller through a needle in your hand or arm
- Injections into your bottom (this is quite rare)
- Painkilling suppositories into your rectum (back passage)
- Tablets when you are able to drink again.
How long will I need to stay in hospital?
If your procedure is carried out laparoscopically, you will most likely be discharged the same day or next day. Some patients will need to stay in the hospital longer. This will all be explained should this situation arise.
If you have laparoscopic cholecystectomy and common bile duct exploration at the same time, you will require a longer hospital stay, which will be discussed with you.
If you have an open operation, you will usually need to stay in hospital for 2 – 3 days. Plans for your discharge from hospital will be discussed with you before any decisions are made.
When you are ready to go home, you will be given a copy of your discharge plan, which gives details of any arrangements made for you, for example, if you need to see your GP, practice nurse or district nurse to have stitches removed or dressings changed. A copy will also be sent to your GP.
Please ask your nurse if you need a fit note.
Simple painkillers will be given to you to take home. Any medications that you need to take will be explained to you.
When can I return to work?
This will depend upon the type of work you do and type of the procedure you had. Your surgeon will advise at the time of your discharge.
*Ask your GP for further advice*
What will happen after I am discharged from hospital?
You will not be given a follow-up appointment. Please contact the Surgical Decisions Unit within 1 week of your discharge from hospital if you have:
- Pain which is not helped with simple painkillers
- A high temperature or feel feverish
- Jaundice (yellow discolouration of your skin)
- Dark coloured urine
- Cream/green coloured discharge from a wound.
After 1 week, please seek advice from your GP.
Contact numbers
If you have any problems following your discharge from hospital please contact.
University Hospital of North Tees
Surgical Decision Unit
Telephone: 01642 624566 or 01642 624628
Monday to Friday, 8.00am to 8.00pm
Saturday to Sunday, 8.00am to 4.00pm
Further information is available from:
NHS Choices
Telephone: 111 (when it is less urgent than 999) Calls to this number are free from landlines and mobile phones or via the website at www.nhs.uk
References/Further Reading
- Inadvertent perioperative hypothermia, National Institute for Health and Care Excellence (NICE), 2008 [updated 2016]. Clinical guideline 65.
- Chole Study Group, West Midlands Research Collaborative, & McNair, A (2016). Population-based cohort study of outcomes following cholecystectomy for benign gallbladder diseases. British Journal of Surgery, 103(12), 1704-1715. DOI: 10.1002/bjs.10287 ¹
- Sathesh-Kumar T, Saklani AP, Vinayagam R (2004). Spilled gall stones during laparoscopic cholecystectomy: a review of the literature. Post Graduate Medical Journal, (80) 77-79 ²
- https://www.bsg.org.uk/clinical-resource/updated-guideline-on-the-management-of-common-bile-duct-stones-cbds/ British Society of Gastroenterology 2016
- https://publishing.rcseng.ac.uk/doi/full/10.1308/rcsann.2020.0109, Intraoperative laparoscopic ultrasound for suspected choledocholithiasis; 2020
- https://academic.oup.com/bjs/article/108/12/1506/6395095 Intervention versus surveillance in patients with common bile duct stones detected by intraoperative cholangiography: a population-based registry study
- https://easl.eu/wp-content/uploads/2018/10/Gallstones-English-report.pdf Clinical Practice Guidelines on the prevention, diagnosis and treatment of gallstones , European Study of liver disease ( EASL) 2018
- https://wjes.biomedcentral.com/articles/10.1186/s13017-022-00456-6 Consequences of the spilled gallstones during laparoscopic cholecystectomy: a systematic review 2022
Patient Experience Team (PET)
Comments, concerns, compliments or complaints
We are continually trying to improve the services we provide. We want to know what we’re doing well or if there’s anything which we can improve, that’s why the Patient Experience Team (PET) is here to help. Our Patient Experience Team is here to try to resolve your concerns as quickly as possible. The office is based on the ground floor at the University Hospital of North Tees if you wish to discuss concerns in person. If you would like to contact or request a copy of our PET leaflet, please contact:
Telephone: 01642 624719
Freephone: 0800 092 0084
Opening hours: Monday to Friday, 9:30am to 4:00pm
Email: [email protected]
Out of hours
Out of hours if you wish to speak to a senior member of Trust staff, please contact the hospital switchboard who will bleep the appropriate person.
Telephone: 01642 617617
Data protection and use of patient information
The Trust has developed Data Protection policies in accordance with Data Protection Legislation (UK General Data Protection Regulations and Data Protection Act 2018) and the Freedom of Information Act 2000. All of our staff respect these policies and confidentiality is adhered to at all times. If you require further information on how we process your information please see our Privacy Notices.
Telephone: 01642 383551
Email: [email protected]
Privacy NoticesLeaflet feedback
This leaflet has been produced in partnership with patients and carers. All patient leaflets are regularly reviewed, and any suggestions you have as to how it may be improved are extremely valuable. Please write to the Clinical Governance team, North Tees and Hartlepool NHS Foundation Trust, University Hospital of North Tees, TS19 8PE or:
Email: [email protected]
Leaflet reference: PIL1452
Date for Review: September 2026