Information for patients
This leaflet can be made available in other formats including large print, CD and Braille and in languages other than English, upon request.
This leaflet tells you about Bronchiolitis.
Most babies or young children who have bronchiolitis are not seriously ill and make a full recovery. Sometimes, if it becomes more serious, your baby or child may need to be admitted to hospital.
What is bronchiolitis?
Bronchiolitis is an infection of the small airways in the lung (the bronchioles). It is common in babies under the age of 1 year.
Bronchiolitis is caused by a virus called Respiratory Syncytial Virus (RSV). This virus is passed by being close to someone who is coughing and sneezing. In most babies and young children, the virus causes only a mild infection like a common cold, but occasionally it can cause a more serious infection of the respiratory tract (airways).
Although RSV is present throughout the year, it most commonly causes infections during the winter months.
What is the respiratory system?
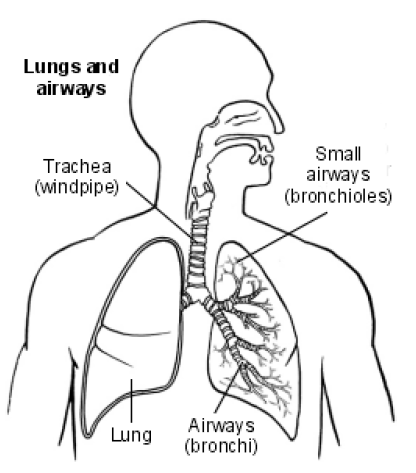
Air travels into the lungs through the trachea (windpipe), down bronchi (large branching airways) and into bronchioles (smaller airways).
The bronchioles are the smallest airways before the air enters the alveoli (millions of tiny air sacs) of the lung. Oxygen from the air passes into the bloodstream through the walls of the alveoli.
What are the symptoms?
At first your baby or young child may have symptoms like a common cold:
- A slight fever, above 37.5oC (99.5oF).
- A snuffly or runny nose which becomes worse in the evenings.
- A mild cough.
- Breathing more rapidly (quickly) and more shallow than usual.
After 2 to 3 days, the symptoms may become more severe and your baby or young child may:
- Have increased difficulty breathing.
- Develop a troublesome cough which may cause vomiting (being sick).
- Become breathless and may sound wheezy.
- Breathe more rapidly, nostrils may flare and you may see the muscles under their ribs sucking in with each breath.
- Seem tired and sleep more or become more unsettled.
- Not be interested in feeding or take less feed.
- Have fewer wet nappies.
What tests can be done?
A Doctor will listen to your child’s lungs using a stethoscope. They may collect some of the mucus (thickened fluid) from your child’s nose and send it to a laboratory for testing to see which virus or a bacterium (germ) is causing the illness.
What is the treatment?
Most babies and young children with this illness can be cared for at home and make a complete recovery in a few days.
There is no medicine to treat Bronchiolitis.
If your baby or child’s symptoms become more severe, or if they have other health problems, your GP may suggest admission to hospital.
In hospital, staff can monitor (check) your baby or child’s condition very carefully. If needed, oxygen can be given to help with their breathing and this may be needed for a few days.
In very severe cases, your baby or child may need help with their breathing (assisted ventilation) until the infection goes. Your baby or child may need to be moved to a different ward or hospital for specialist help.
Before feeds, staff may remove any mucus from your baby or child’s nose using gentle suction (sucking out) through a fine tube. This will help make feeding easier. Suction is not always needed.
IF your baby or child is not able to drink at all they may need to be given either:
- Feeds or special fluids through a nasogastric tube (a small tube) passed through their nose into their stomach.
- Special fluids through a cannula (a fine tube) inserted into a vein in the back of their hand, arm or foot using a small, fine needle. This is called an intravenous drip.
When your baby or child is able to feed and breathe more easily and no longer needs extra oxygen you will be able to take them home.
How long will the illness last?
This illness often becomes worse over 3 to 5 days before your baby or child starts to get better. It can last for about 2 to 3 weeks. A cough and wheeze may last for a few more weeks in some babies and children. Children can also develop a wheeze with future coughs and colds.
How can I help my baby or child to recover?
It is very important that no one smokes in your home or around your baby or child. Breathing smoky air will make them cough and become breathless again. Smoking can affect and harm a baby or young child’s lungs, which are still developing.
Your baby or child should be kept in a warm and well-aired room.
It is recommended that you do not take your baby/child outdoors until they are fully recovered, where possible.
If your baby or child develops problems feeding or breathing you must contact your GP as soon as possible.
Reducing feed amounts, giving smaller feeds more frequently may help.
You can give your baby or child Paracetamol (for example, Calpol).
You must always follow the instructions provided in the leaflet supplied with your medicine. If you are not sure, ask your Pharmacist what is suitable for your baby or child and what dose you should give.
Will my child get RSV again?
Although a baby or child can catch further RSV infections usually, the symptoms will be much milder than the first time.
You can help to prevent future spread of the virus by using a tissue to cover your nose and mouth when coughing, sneezing or wiping your nose, and carefully disposing of tissues and washing your hands afterwards.
Washing of hands plays a big part in preventing the spread of viruses and infections.
You should try to keep new-born babies away from people with colds or flu.
Contact numbers
If you have any worries or concerns you should contact:
Children’s Ward
Telephone: 01642 382 815
24 hours a day, 7 days a week.
Children’s and Young Person’s Emergency Department
Telephone: 01642 624 533
24 hours a day, 7 days a week.
If you have any worries or concerns you should contact your GP during normal surgery hours. Outside surgery hours, you should contact your GP’s surgery for the Out of Hours Service number or attend a walk in centre.
Further information is available from:
NHS Choices
Telephone: 111 (when it is less urgent than 999)
Calls to this number are free from landlines and mobile phones or via the website at www.nhs.uk
Patient.co.uk
https://patient.info/chest-lungs/bronchiolitis-leaflet
NHS Choices
www.nhs.uk/Conditions/Bronchiolitis/Pages/Introduction.aspx
Comments, concerns, compliments or complaints
Patient Experience Team (PET)
We are continually trying to improve the services we provide. We want to know what we’re doing well or if there’s anything which we can improve, that’s why the Patient Experience Team (PET) is here to help. Our Patient Experience Team is here to try to resolve your concerns as quickly as possible. The office is based on the ground floor at the University Hospital of North Tees if you wish to discuss concerns in person. If you would like to contact or request a copy of our PET leaflet, please contact:
Telephone: 01642 624719
Freephone: 0800 092 0084
Opening hours: Monday to Friday, 9:30am to 4:00pm
Email: [email protected]
Out of hours
Out of hours if you wish to speak to a senior member of Trust staff, please contact the hospital switchboard who will bleep the appropriate person.
Telephone: 01642 617617
Data protection and use of patient information
The Trust has developed Data Protection policies in accordance with Data Protection Legislation (UK General Data Protection Regulations and Data Protection Act 2018) and the Freedom of Information Act 2000. All of our staff respect these policies and confidentiality is adhered to at all times. If you require further information on how we process your information please see our Privacy Notices.
Telephone: 01642 383551
Email: [email protected]
Privacy NoticesLeaflet feedback
This leaflet has been produced in partnership with patients and carers. All patient leaflets are regularly reviewed, and any suggestions you have as to how it may be improved are extremely valuable. Please write to the Clinical Governance team, North Tees and Hartlepool NHS Foundation Trust, University Hospital of North Tees, TS19 8PE or:
Email: [email protected]
Leaflet reference: PIL1133
Date for Review: January 2027