Information for patients
This leaflet can be made available in other formats including large print, CD and Braille and in languages other than English, upon request.
This leaflet covers the first few weeks after your injury when your arm is in a sling.
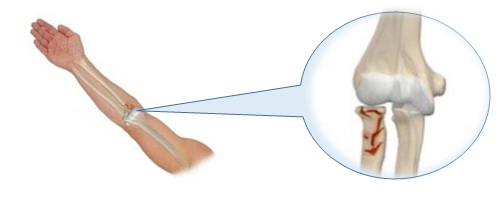
What is a radial head or radial neck fracture?
A fracture is when your bone breaks, this can be a thin crack to completely broken bone.
The radius is one of the bones in your forearm. A fracture to the radial head or neck occurs near the elbow joint. This usually happens when falling on an outstretched arm.
What to expect following the fracture?
These fractures normally take between 6 to 12 weeks to heal, and full recovery can take up to six months. However, it could be longer, as this type of fracture is linked to stiffness of the joint.
Following this type of injury, the main aim is to regain enough movement to perform day-to-day activities. No forceful stretching should be performed at any time during your rehabilitation.
Early mobilisation of the elbow should be encouraged to minimise the risk of developing elbow stiffness. Simple exercises can be done to to help with your recovery.
The following exercises can be done immediately after your injury. Try to complete 3 sets of 15 repetition (45 times with short pauses every 15), twice per day.
Exercise 1 – Table Slides


Start sitting or standing with the arm/hand supported on the counter top or table. Slowly slide your arm in front until you feel a stretch. se a towel or similar to reduce friction.
Exercise 2 – Active Assisted Supination/Pronation


Sit up straight in a chair with your forearm supported on a table. With your elbow straight, turn your palm up to face the ceiling, then down to face the table, as much as possible turning only the forearm.
Exercise 3 – Active Hand Pumps


Hold your hands in front with your fingers straight and spread apart. Close your hands into a fist and then open and spread your fingers. Each repetition should take 3 seconds.
It is more effective to do small amounts of repetition regularly throughout the day. This should mean your exercises are manageable and your arm does not stiffen up between sets.
Is there anything I can do to help myself?
Stay focused on your exercises. If you notice any new swelling, redness or increased pain, contact your GP. Factors like stopping smoking, controlling alcohol intake and management of diabetes play a significant role in effective healing. These factors increase inflammation in our bodies, which unfortunately reduces our ability to undergo effective healing. For further advice, please see useful links section.
What advice is there for using a sling?
Following the identification of the fracture, you will be issued with a sling from the orthopaedic department at your appointment and advised regarding how to use it and the length of time you will be expected to wear it. The sling should be worn for comfort initially unless otherwise specified. The length of time needed for using a sling will vary from patient to patient, but this will be discussed with you by a member of the orthopaedic team.
You can remove the sling for washing, eating, changing of clothes, and when doing your exercises.
If you have not injured your shoulder, wrist or hand of the affected arm, it is safe and important to move them regularly. This will help prevent stiffness, reduce swelling and maintain the function of the arm.
What medication can I take for pain relief?
When you have fractured a bone, it can be very painful. Pain medication will not help the bone heal faster; however, it may help make you more comfortable while the bone heals.
There are many different pain medications you can take. Sometimes a simple over the counter pain medication such as paracetamol can work. Simply follow the instruction on the box. However if you are in a lot of pain you may need something stronger, for this you will need a prescription from your GP.
Is there any medication that should be avoided?
There is some evidence which tell us that some anti-inflammatory medicines such as ibuprofen and naproxen can slow the fracture from healing. It is best to limit, where possible, taking anti-inflammatory medication as to not slow down the healing process.
Frequently Asked Questions (FAQ)
What advice is there to help with dressing?
It is easier to use front button shirts and pull-up trousers with an elastic waistband in the first few weeks. When dressing put the injured arm into sleeves first and when undressing take the un-injured arm out first, followed by the injured arm.
How do I sleep?
You may find it easier to sleep more upright than usual, using pillows to prop you up in bed or in a reclining armchair. These injuries are usually very sore, and you may need to take pain relief, especially in the first two weeks or when you do your exercises. Follow the instructions on the box.
When can I drive?
There is no set timescale of when you can drive; it will be different for each individual. You can return to driving once you are no longer using your sling, and you have adequate strength and range of movement at the shoulder in order to control the car safely and comfortably. You should also ask yourself if you would be able to perform an emergency stop if needed. Most people feel safe to do this around 6 to 8 weeks. You may need to inform the DVLA of your injury.
When can I return to work?
You may need to take some time off work. The doctors in fracture clinic or your GP can sign you off. You can return to work as soon as you feel and are able to perform your normal duties. For manual work, you may not be able to return for 3 months but if you can perform light duties this may be from 6 weeks depending on your own pain and mobility in the arm.
When can I return to leisure activities?
This will vary dependent on your pain, range of movement and strength in your shoulder. You should avoid heavy lifting for approximately 12 weeks. You can return to sports with guidance from your Physiotherapist. Usually you can restart lighter sport 6 weeks after your injury and contact sports after 12 weeks. You should also remember to pace yourself and not try to do everything all at once – little and often is better.
Contact Details
University Hospital of North Tees
Orthopaedic Outpatients
Telephone: 01642 624 486
University Hospital of Hartlepool
Orthopaedic Outpatients
Telephone: 01429 522 590
Physiotherapy Appointment Queries
Telephone: 01429 522 471
Monday to Friday, 09:00 a.m. to 04:30 p.m.
Other Useful Links
- Make Every Contact Count Gateway
MECC – https://www.meccgateway.co.uk/nenc
- North tees and Hartlepool NHS foundation trust
Stop Smoking Service – https://www.nth.nhs.uk/services/stop-smoking-service/
- NHS live well – Healthy weight
Advice and education on weight loss and maintain a healthy weight – https://www.nhs.uk/live-well/healthy-weight
Comments, concerns, compliments or complaints
Patient Experience Team (PET)
We are continually trying to improve the services we provide. We want to know what we’re doing well or if there’s anything which we can improve, that’s why the Patient Experience Team (PET) is here to help. Our Team is here to try to resolve your concerns. The office is based at the University Hospital of North Tees if you wish to discuss concerns in person. Our contact details are:
Telephone: 01642 624719
Freephone: 0800 092 0084
Opening hours: Monday to Friday, 9:30am to 4:00pm
Email: [email protected]
Out of hours
Out of hours if you wish to speak to a senior member of Trust staff, please contact the hospital switchboard who will bleep the appropriate person.
Telephone: 01642 617617
Patient, Public and People with Lived Experience
We are looking for patients to share their experiences of healthcare and to join our Involvement Bank. Working with the patients, carers, families and the general population we support in making decisions about their care can lead to better health outcomes, increased patient satisfaction and a better overall experience. We want to listen and work with you in shaping the future of your healthcare services. To find out more about the Involvement Bank go to our website or contact us at:
Website: www.nth.nhs.uk/about/community/people-with-lived-experience
Email: [email protected]
Data protection and use of patient information
The Trust has developed Data Protection policies in accordance with Data Protection Legislation (UK General Data Protection Regulations and Data Protection Act 2018) and the Freedom of Information Act 2000. All of our staff respect these policies and confidentiality is adhered to at all times. If you require further information on how we process your information please see our Privacy Notices.
Telephone: 01642 383551
Email: [email protected]
Privacy NoticesLeaflet feedback
This leaflet has been produced in partnership with patients and carers. All patient leaflets are regularly reviewed, and any suggestions you have as to how it may be improved are extremely valuable. Please write to the Clinical Governance team at:
Email: [email protected]
Leaflet reference: PIL1558 – Version 01
Date for Review: 16/06/2028