Information for patients
This leaflet can be made available in other formats including large print, CD and Braille and in languages other than English, upon request.
What is Obstructive Defaecation Syndrome (ODS)?
During a normal bowel movement, all the muscles inside your pelvis, including the anal sphincter (the ring of muscle just inside your bottom that opens and closes your bowels) must relax in order to allow passage of faeces (poo) out of the body. Sometimes, these muscles fail to relax or they can even squeeze (contract) instead of relaxing.
This can cause the following symptoms:
- Difficulty in opening your bowels. You could experience straining or the inability to pass poo.
- The feeling of not having “finished” on the toilet and not having completely emptied your bowel (called tenesmus).
- Feeling of blockage or obstruction in your back passage.
- Needing to use a finger to help get the poo out.
What causes ODS?
It may be due to:
- Poor toileting habits, for example, delaying the “need to poo”, or regular straining.
- Issues after childbirth, tear, or open sore that develops in the opening of the back passage.
- Back pain.
- Psychological distress such as previous sexual or physical abuse.
- Eating disorders.
- Neurological disorders such as Parkinson’s disease.
What tests might I have?
The management of (ODS) mainly involves the treatment and management of symptoms. This will include lifestyle advice and biofeedback techniques (a bowel treatment programme) that are taught in the clinic by your nurse specialist.
Your specialist may advise that you take some tests to help you get a clear diagnosis. These may include any or all of the following:
- Blood tests.
- Anorectal physiology (manometry) – is a way of measuring how well the muscles of your lower part of the bowels are working. If you need this test, you will be given a leaflet about it.
- Endo–anal ultrasound – this scan will look at your anal sphincter (back passage muscle) to check if there are any defects.
- Defaecating Proctogram – This is an examination of the lower bowel and rectum using X-rays. It shows how your rectum functions while you have a poo.
- Flexible Sigmoidoscopy/Colonoscopy – these are camera tests on the bowel to see if there are any abnormalities.
Which muscles are involved in a normal bowel movement?
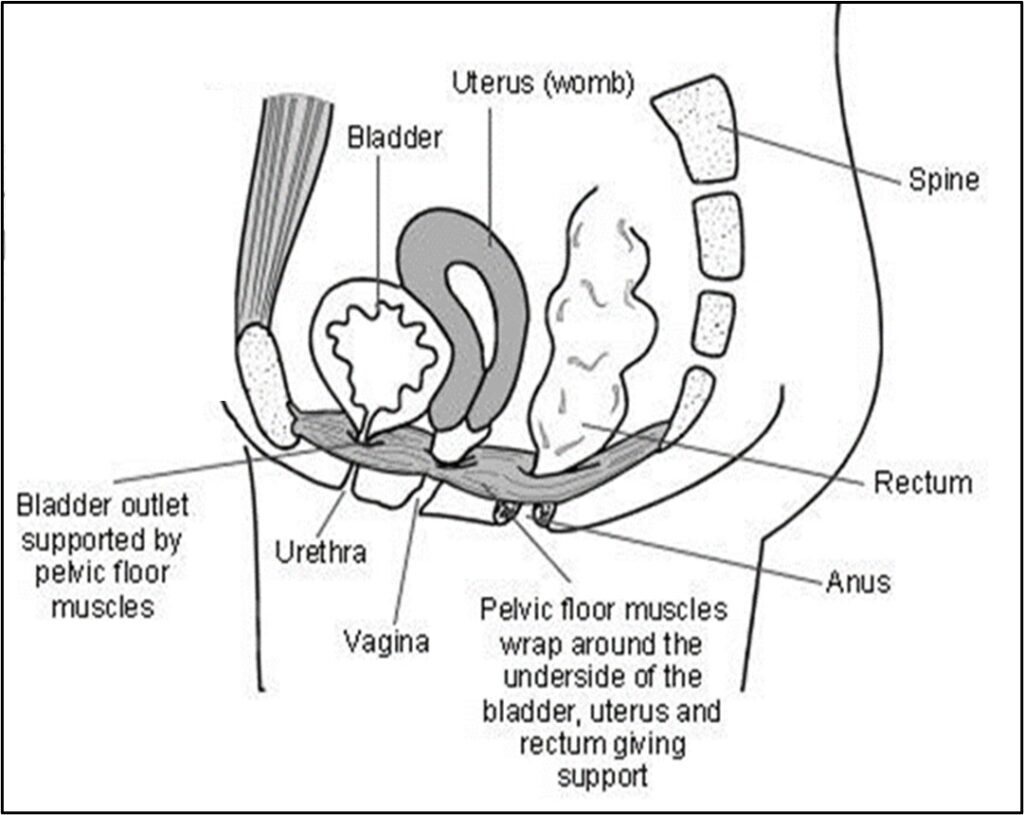
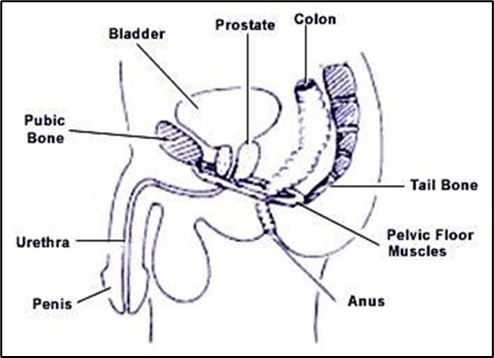
When you open your bowels the pelvic floor muscles and the muscles of your back passage, called the external anal sphincter, relax to enable the bowel to open. The pelvic floor muscles form a hammock that runs from your pubic bone at the front, to your coccyx (tailbone) at the back, and help to support your pelvic organs.
One of the pelvic floor muscles is called the puborectalis. This forms a U-shaped sling around the back passage. When it is tight and not relaxed it pulls the anal canal forward and creates a bend in it called the anorectal angle, making it harder to pass poo. When you need a poo, certain muscles in your pelvic floor should relax. If they do not relax, you might find it difficult to poo. This might mean you have to learn how to relax the muscles.
What can I do to help myself?
A general advice is to eat a healthy diet high in fruit, vegetables and fibre and drink plenty of water. This will help to keep your poo soft and easy to pass. You can also try the following exercises:
Exercises
When not on the toilet
- Pelvic floor relaxation breathing technique: Lie down with your knees bent and feet flat on the floor. Breathing fully, hold your breath and consciously relax your abdomen outwards and downwards. Then sigh the breath out, imagining your pelvis is getting wider as you do so. Repeat 5 times.
- Child’s pose with open knees: Kneel down with wide knees (so that your tummy can drop in between your knees) and put your forehead on the ground and your arms above your head. Relax fully, feeling the stretching of your pelvic muscles. Remain in this position for 5 minutes if you can.

- Side twist/thoracic expansion: Lie down on your side with your knees bent and arm stretched out in front of you. Then bring one arm over to the other side and roll onto your back, keeping your knees in the same position. Hold the stretch for 2 minutes, then roll over onto the opposite side and repeat on the opposite side.

- Try perineal massage: Wash your hands and keep your nails short. Using a lotion or lubricant suitable for intimate areas, gently massage your perineum (the area between your scrotum and anus if you are a man or your vagina and anus if you are a woman). This will help the muscles in that area to relax.
When sitting on the toilet
- Keep your knees higher than your hips when sitting on the toilet, by putting a small footstool underneath your feet. This makes the anal canal straighter and therefore making it easier to open your bowels.

- Try the “wonder woman” pose: Sit with your feet apart and hands on your hips. Push your tummy out until you feel it pushing against your fingertips. This will automatically relax your pelvic floor muscles.
Do you have any questions?
This information leaflet is designed to inform you about (ODS). If you do not understand any part of this information, ask your doctor, nurse or physiotherapist for help.
Contact Numbers
If you need further advice or have any problems, please contact the colorectal unit.
University Hospital of North Tees
Colorectal Unit
Telephone: 01642 624399
Monday to Friday, 8:00 am to 4:00 pm
Further Information
- Bladder & Bowel Health – Bowel & Bladder UK.
Website: https://www.bbuk.org.uk/adults/
- Good Bowel Health – Pelvic Obstetric & Gynaecological Physiotherapy (POGP).
Website: http://https//thepogp.co.uk/patients/pelvic_health_advice/bowel_health.aspx
- Nurse and Physiotherapy Led Pelvic Floor Biofeedback Unit – St. Mark’s National Bowel Hospital
Website: https://www.stmarkshospital.nhs.uk/services-a-z/biofeedback/nurse-and-physiotherapy-led-pelvic-floor-biofeedback-unit/
Comments, concerns, compliments or complaints
Patient Experience Team (PET)
We are continually trying to improve the services we provide. We want to know what we’re doing well or if there’s anything which we can improve, that’s why the Patient Experience Team (PET) is here to help. Our Team is here to try to resolve your concerns. The office is based at the University Hospital of North Tees if you wish to discuss concerns in person. Our contact details are:
Telephone: 01642 624719
Freephone: 0800 092 0084
Opening hours: Monday to Friday, 9:30am to 4:00pm
Email: [email protected]
Out of hours
Out of hours if you wish to speak to a senior member of Trust staff, please contact the hospital switchboard who will bleep the appropriate person.
Telephone: 01642 617617
Patient, Public and People with Lived Experience
We are looking for patients to share their experiences of healthcare and to join our Involvement Bank. Working with the patients, carers, families and the general population we support in making decisions about their care can lead to better health outcomes, increased patient satisfaction and a better overall experience. We want to listen and work with you in shaping the future of your healthcare services. To find out more about the Involvement Bank go to our website or contact us at:
Website: www.nth.nhs.uk/about/community/people-with-lived-experience
Email: [email protected]
Data protection and use of patient information
The Trust has developed Data Protection policies in accordance with Data Protection Legislation (UK General Data Protection Regulations and Data Protection Act 2018) and the Freedom of Information Act 2000. All of our staff respect these policies and confidentiality is adhered to at all times. If you require further information on how we process your information please see our Privacy Notices.
Telephone: 01642 383551
Email: [email protected]
Privacy NoticesLeaflet feedback
This leaflet has been produced in partnership with patients and carers. All patient leaflets are regularly reviewed, and any suggestions you have as to how it may be improved are extremely valuable. Please write to the Clinical Governance team at:
Email: [email protected]
Leaflet reference: PIL1579 – Version 01
Date for Review: 20 October 2028