Information for patients
This leaflet can be made available in other formats including large print, CD and Braille and in languages other than English, upon request.
Critical Care Philosophy
Our philosophy of care is to provide clinical excellence for all patients who experience a critical illness throughout the hospital.
Introduction
Approximately 100,000 patients are admitted to Intensive Care in the UK every year. For patients and relatives this can be a frightening experience, and you may find it difficult to cope at times. Though some admissions are planned, most are not, and it is quite usual to feel worried and upset.
We aim to provide practical information and advice on what to expect. We understand the information you are given may be overwhelming and forgotten at such a difficult time. We hope this booklet will be a help for you to take away and refer to later.
Why are people admitted to Critical Care?
Critical Care Units are specialised areas within a hospital. We look after patients whose condition is life-threatening and need constant, close monitoring and support from equipment and medication.
There are many reasons why people may need care in Critical Care. These range from a planned admission following a major operation, to emergencies from sudden illness or accidents.
Critical Care Units are run and staffed by specialist doctors and nursing staff who have undergone extensive training. Our staff will manage patients admitted to the Unit, with involvement of other specialists as needed.
Welcome to the Unit
North Tees Critical Care Unit is a mixed general Intensive Care Unit (ICU) and High Dependency Unit (HDU) which has 17 beds.

The Critical Care Unit is divided into 3 areas:
- Unit A (4 beds)
- Unit B (9 beds)
- Unit C (4 beds)
You will find staffing levels are higher than the normal ward so one nurse will look after one or two patients. Doctors are always present on the Unit. There is always at least one consultant on duty to ensure patients have immediate access to a senior medical opinion.
All staff wear an identification badge which includes their name, job title and a photograph. Please do not hesitate to ask staff to show you their identification badge. All staff should introduce themselves to you.
What happens on admission?
When your relative is admitted we need to assess their immediate needs, stabilise their condition and make them comfortable. In order to do this we may need to insert various devices and tubes and attach them to our equipment. This can take some time: from 20 minutes to over 1 and a half hours. This may mean you cannot visit for some time after your relative is admitted.
We realise you will be anxious to see your loved one and it can be frustrating waiting for news. We aim to keep you informed of progress and will allow you to visit as soon as possible. It is important we have as much personal information as possible about each patient.
The nurse at the bedside may well have as many questions for you as you have for them. It is important we know about your relative or loved one so we can understand their needs more fully.
We aim to offer relatives the time to discuss patient care with the duty Consultant, or a senior member of the medical team.
What should I expect when arriving at the Unit?
The Critical Care Unit is situated on the first floor, Ward 20. There is a buzzer you will need to ring to alert the staff that you are waiting to enter. The doors are locked for patient safety. You will be asked to enter, stand back from the doors as they open outwards.
On entry you will find a reception hatch on your left. Team support staff can check if it is appropriate for you to go into the Unit.
When you enter the Unit for the first time there is a lot to take in. The environment is noisy and can be overwhelming, and your relative may be connected to monitors, drips and machines.
Every patient is attached to a heart monitor. This continually displays the heart rate, blood pressure and oxygen saturation for patient safety and to guide our treatment.
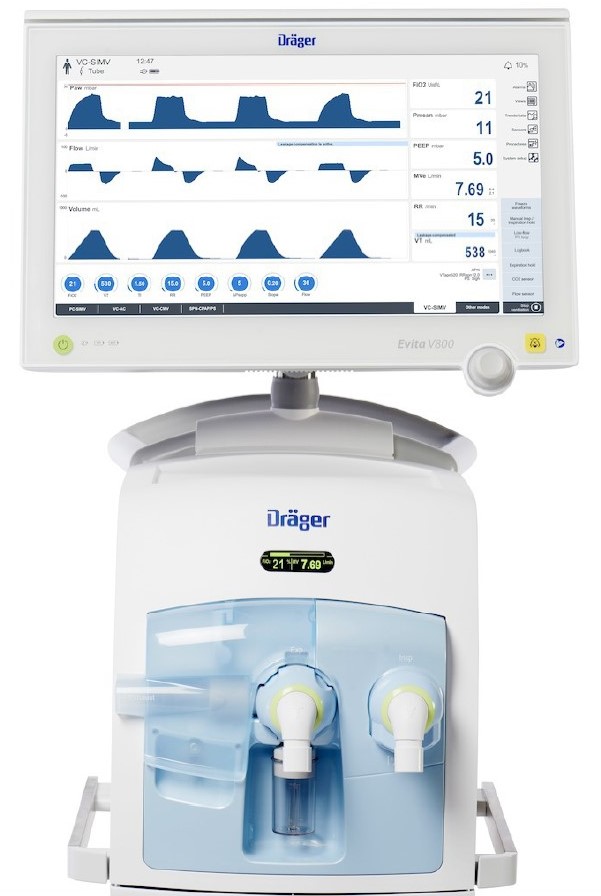
Some patients are attached to breathing machines (ventilators) via tubes in their mouths to assist their breathing. There might also be kidney machines (haemofilters) which are attached to a large tube into the blood stream.


Alarms are set on monitors and other equipment by the nurse at the bedside and you may hear buzzers and alarms sounding. Please do not worry, they are just telling the nurse that something needs attending to.
Patient information and confidentiality
The Critical Care Unit is an environment with rapidly changing patient conditions. We endeavour to provide you with timely information about your loved one’s condition. Conditions can change in between contact and we can only give information relevant at that particular time.
If you would like to make enquiries about your family member’s progress while they are in Critical Care it would help if you could ask only one member of your family to contact the Unit. They can then pass on the information to the rest of your family.
We respectfully ask you to avoid telephoning during nurse handover times which are 7.15 to 7.45 both morning and evenings. For patient privacy and confidentiality, only brief information will be given over the phone.
Car parking facilities
There are several car parking facilities on the hospital grounds and local surrounding area; cost to park vary. Please ensure you have a valid parking ticket at all times and valid for the area you choose to park your vehicle.
Please speak to Critical Care reception staff for information to see if you qualify for any parking concessions.
Security office near the main entrance of North Tees Hospital can also advise on parking facilities and any concessions that may be available to you.
e.g. Weekly parking ticket, Blue Badge Holder .
What are the visiting times?
The visiting times for our Unit are 12:30 p.m. to 2:30 p.m. and 3:30 p.m. to 6:30 p.m. This is rigid as it is important for the patient to have some quiet time during the day. If you are unable to visit at those specific times then please talk to the nurse at the bedside.
What should visitors be aware of?
Visitors are asked to consider the rights and privacy of all patients.
• Only 2 visitors are allowed at a bedside at any one time.
• Anyone making too much noise may upset other patients and may be asked to leave.
• You may need to leave the bedside if unit staff ask you to.
• Hospital property should be respected and not abused or damaged.
• You should not visit patients if you have signs of an infection, for example, a cold, sore throat, tummy bug or you are generally unwell.
• You should not sit on the bed during visits.
• Mobile telephones must not be switched on or used in or near any clinical treatment areas to maintain patient and staff confidentiality. Mobile phones should be switched to flight mode or silent mode or locked in a relative locker.
Mobile phones may be used by clinical staff members these are specifically provide for staff by the Trust to speak with other team members to co-ordinate appropriate care for your loved one.
While we will support your visiting needs, our prime focus is on the care of your relative or friend. For this reason it may be necessary to interrupt your visit and ask you to leave the bedside temporarily. This is so personal care, position changes or medical interventions can take place.
We understand this can be frustrating, particularly if you have limited time available to visit. However, we ask you to bear with us.
Visiting can be emotional and exhausting for both visitor and patient. It is important you get lots of rest, drinks and meals. It is important you look after yourself so you are strong when your relative needs you.
We have one visitors’ lounge for the unit situated just outside of the Unit. There is a toilet, tea and coffee making facilities and a TV. We have a counselling room on the Unit which is used for visitor discussions with the medical staff.
How can I help prevent infection?
Patients who are critically ill may have difficulty fighting infections. Staff will do all they can to make sure your relative or friend is protected.
You can help by:
• Cleaning your hands with soap and water and use alcohol gel every time you enter or leave the Unit.
• Wearing a plastic apron every time you enter the Unit.
• Placing any personal property (such as bags, mobile phone) and coats in the lockers available inside the Unit. A £1 coin or trolley coin can be used and is returned when opening the locker.
How can I help on the Unit?
Your relative may be unconscious as a result of their illness or the drugs given to them to keep them comfortable.
They may be able to hear you even if they cannot respond. Although it may feel strange, talk to them normally to let them know you are there. They are more likely to recognise or respond to a familiar voice and will draw comfort from your presence. You will notice the nurse talking to your relative explaining what they are doing.
Do not be afraid to touch your loved one. Though the equipment and tubes may be daunting, remember they are still the person you know underneath. You may wish to hold their hand; the nurse will show you how to do this safely.
What do I need to bring into hospital?
Space on the Unit is limited so whilst your loved one is unwell we do not need any personal belongings in the bed space. We initially provide toiletries.
It is easier for the patient to wear one of our gowns as there are many wires and infusions attached. Fresh flowers are not allowed on the Unit for infection control reasons.
Please bring any health passports you have been given, for example, ‘Patient Passport’ for patients with learning disabilities, ‘This is me’ Dementia Passport, or the Integrated Catheter Care Passport. This will help us to give the care needed.
Please note that University Hospital of North Tees does not accept any responsibility for the loss or damage to any personal property.
Patient Diaries
We have developed a patient diary which will be completed daily by the nurse, the doctor and yourself. A diary can be very useful later on to help the person who has been ill. They may have very confused memories of their time in critical care or no memories at all. A diary can help them to understand what happened to them and fill the gaps in their memory.
What if I do not speak or understand English?
We respect your privacy and dignity as well as your religious and cultural beliefs during your treatment and care. All our information can be provided in other formats including large print, CD and Braille, and in languages other than English, upon request.
If you need the services of a professional interpreter or someone who can use sign language please let us know, so this can be arranged.
Spiritual Support
Hospital chaplains provide for the spiritual and religious needs of patients, relatives, visitors and staff. If you would like to see a hospital Chaplin, your own minister or faith leader, please let us know.
The hospital has a Chapel and Multi-Faith Room, located on the ground floor. These facilities provide a tranquil place for quiet reflection or prayer. They are open day and night and cater for people of all faiths.
How can I help improve healthcare?
Healthcare staff are always trying to improve patient care and treatments and part of this process involves research. Research evidence gives healthcare staff information about the latest and best treatments for their patients.
Patients are often too ill to give their consent to enter a study. It is common for a close family member to be asked for this consent. Taking part is entirely voluntary and no one is under any obligation to consent.
Even after consent is given, withdrawal can take place at any time. Should you not wish to take part, this will not affect your treatment or care.
We also contribute data to the Intensive Care National Audit and Research Centre (ICNARC). It provides information and feedback about the quality of critical care.
Moving to a ward?
When your relative is no longer needing specialist care they will be transferred to a ward for further care. It is normal for patients to be fearful at this time.
They have become used to the nurses and other staff on the Unit. It is quite common for you and your loved one to feel vulnerable and apprehensive. This is natural, but please stay positive and see it as progression to normality. You will soon make relationships with the staff on the new ward.
Your relative may not remember much about their time on the Critical Care Unit. Patients might feel stressed and confused about what has happened to them. This is because of their illness, the medication they have been given and lack of proper sleep and rest.
Your relative will rely on you most at this time. You can help them by remaining calm and reminding them of things that are familiar to them. In time you will be able to explain what has happened to them on the Critical Care Unit.
Is there follow-up after discharge?
Once the patient has been discharged to the ward our Outreach Team will visit them on the ward. The Outreach Team is made up of nurses who are part of the Critical Care team.
They can advise the nurses and doctors about the needs of your loved one. They will liaise between the ward and Critical Care for the ongoing care of your relative.
Support Services
The course of critical illness is unpredictable and your relative’s condition may change rapidly. Staff will keep you informed of all important changes. The outcome of serious illness and the response to treatment can be uncertain as everyone is different. The length of stay can vary from as little as a few hours to several weeks.
As long as treatment is continuing to be beneficial, we will continue to support your relative with care to aid their recovery. Sadly, despite all the treatments available some patients are too ill to survive. The death of a loved one is always a devastating event even if it has been expected.
The medical staff on the Critical Care Unit will often be able to warn families that there is deterioration. Death can still happen very suddenly. The doctors and nurses cannot always give a family enough warning to return to the hospital to be present. However, every effort will be made to get you with your loved one at this time
Organ Donation
If treatment is not successful, it is possible you may be asked about organ donation. Organ donation is the gift of an organ or organs to help save the life of someone else who needs a transplant. Most organs can be donated.
Doctors and nurses do everything possible to save lives and organs are only removed for transplantation once all attempts to save life have failed and the patient has died.
Organs are only ever removed for transplantation with the consent of a patient’s nearest relative. These discussions are carried out sensitively and by trained staff.
Tissue Donation – What do I need to do?
If your friend or relative carried a donor card, was on the organ donor register or said they would like to make a donation of organs or tissues this may still be possible up to 24 hours after the death.
If this is something you wish to consider please contact: Tissue Services on 03000 203040. Your details will be taken and a Tissue Co-ordinator will contact you.
Bereavement Support services
The Trust offers Bereavement Support Services. They talk families through the next steps following bereavement. They provide information about coroners, registrars and funeral directors. They help funeral directors with the arrangements for funerals of patients with no family or friends.
What rights do NHS staff have?
We believe all those who work in, or provide services to the NHS have a right to do so without fear of violence or abuse. The NHS nationally is committed to tackling physical and non-physical violence in the workplace and has adopted a national approach to deal with acts of violence on members of staff.
We will not tolerate violence and aggression, including verbal and racial abuse towards staff.
Your Views
Hospital staff will do their best to make sure your relative’s stay is as comfortable as possible and that care is of the highest standard. We always welcome comments about the services we provide and suggestions about how things can be improved.
You can share your experience of our services on NHS Choices. Visit the NHS Choices website at www.nhs.uk and type in which hospital you visited. Your comments help us improve things for future patients.
Contact Numbers
University Hospital of North Tees
Critical Care Unit
Telephone: 01642 382720 or 01642 382820
24 hours a day, 7 days a week
Further information is available from:
- Intensive Care Society (ICS) is dedicated to furthering education and research into intensive care in the UK www.ics.ac.uk
- Headway aims to promote understanding of all aspects of brain injury. It provides information, support and services to people with a brain injury, their families and carers. Helpline: 0808 800 2244 Website: www.headway.org.uk
- ICNARC is dedicated to improving intensive care treatment and helping patients to get better sooner, with fewer complications. Website: https://www.icnarc.org/
- Cruse Bereavement Care provides counselling, support, information, advice, education and training services to the friends and relatives of someone who has died, to help them understand their grief and cope with their loss. Helpline: 0844 477 9400, Young person’s helpline: 0808 808 1677 Website: https://www.ataloss.org/FAQs/cruse-bereavement-care-tees-valley
- The Citizens Advice service helps people deal with their legal, money and other problems by providing free, independent and confidential advice. Website: www.citizensadvice.org.uk
- Carers UK offer support and a sharing of experiences for carers. Website: www.carersuk.org
- ICU Steps is the United Kingdom’s only support group for people who have been affected by critical illness. Website: http://icusteps.org/
Comments, concerns, compliments or complaints
Patient Experience Team (PET)
We are continually trying to improve the services we provide. We want to know what we’re doing well or if there’s anything which we can improve, that’s why the Patient Experience Team (PET) is here to help. Our Patient Experience Team is here to try to resolve your concerns as quickly as possible. The office is based on the ground floor at the University Hospital of North Tees if you wish to discuss concerns in person. If you would like to contact or request a copy of our PET leaflet, please contact:
Telephone: 01642 624719
Freephone: 0800 092 0084
Opening hours: Monday to Friday, 9:30am to 4:00pm
Email: [email protected]
Out of hours
Out of hours if you wish to speak to a senior member of Trust staff, please contact the hospital switchboard who will bleep the appropriate person.
Telephone: 01642 617617
Data protection and use of patient information
The Trust has developed Data Protection policies in accordance with Data Protection Legislation (UK General Data Protection Regulations and Data Protection Act 2018) and the Freedom of Information Act 2000. All of our staff respect these policies and confidentiality is adhered to at all times. If you require further information on how we process your information please see our Privacy Notices.
Telephone: 01642 383551
Email: [email protected]
Privacy NoticesLeaflet feedback
This leaflet has been produced in partnership with patients and carers. All patient leaflets are regularly reviewed, and any suggestions you have as to how it may be improved are extremely valuable. Please write to the Clinical Governance team, North Tees and Hartlepool NHS Foundation Trust, University Hospital of North Tees, TS19 8PE or:
Email: [email protected]
Leaflet reference: PIL
Date for Review:
