Information for patients
This leaflet can be made available in other formats including large print, CD and Braille and in languages other than English, upon request.
What are pressure ulcers?
Pressure ulcers are areas of damaged skin and flesh. They are also known as bed sores or pressure sores.
They are caused by 2 main things:
- Pressure: The weight of the body or a medical device pressing down on or against the skin.
- Shear: The layers of skin are forced to slide over one another. For example, when you slide down or are moved up the bed or when you are being transferred, such as from a bed to a chair.
Tight clothing or anything that stops you moving easily can also cause problems.
Pressure ulcers can develop very quickly. If you notice any signs or symptoms, you must notify your GP or nurse immediately.
Pressure ulcers usually start with changes to the skin; it may appear red or darker in colour, or feel hot or cold. The redness will not blanch (turn white) when lightly pressed. You may feel pain, tenderness or tingling.
If the cause of the problem is not removed as early as possible then the skin can blister and a deep ulcer can develop. If you do have any of these symptoms then you must tell your nurse or GP, or ask a relative, friend or carer to contact your nurse or GP for you. The nurse or GP will give you advice on what to do next.
Please talk to your nurse if you would like to know more about pressure ulcers.
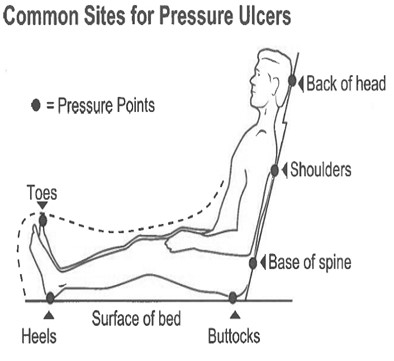
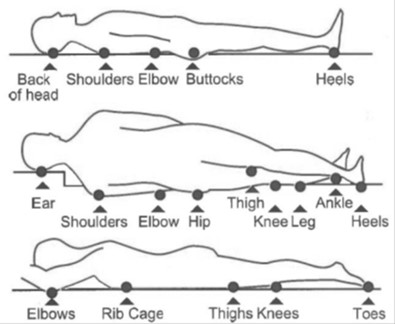
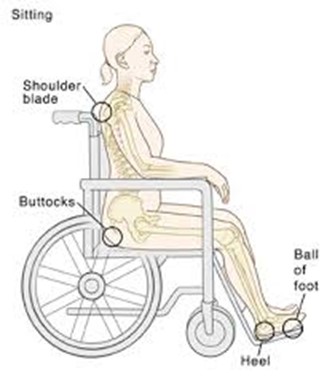
Where do pressure ulcers occur?
You can get a pressure ulcer anywhere on your body. The most common places are those parts of your body which take your weight when you are lying or sitting and where your bone is close to the surface.
For example, your buttocks (bottom), sacrum (base of spine), heels, hips, elbows, ankles, shoulders, spine (back) or back of your head (see diagrams 1, 2 and 3).
Pressure ulcers can also occur anywhere where a device comes into contact with the skin, for example oxygen tubing, facemasks, visors, prosthesis, orthopaedic braces and casts.
Where pressure damage may occur;
Am I at risk of getting a pressure ulcer?
Between 4 to 10 patients in every 100 develop a pressure ulcer in hospital.1 However, it is unknown how many patients in a community and care home setting will develop a pressure ulcer.2
Your body usually protects you from ulcers by telling you to move. If you are unwell or have lost feeling in parts of your body you may not be able to move and will be at risk.
You are more likely to develop pressure ulcers if you:
- Have to stay in bed.
- Are in a wheelchair.
- Cannot move around very well.
- Have a serious illness.
- Are elderly or weak.
- Are incontinent (poor bladder or bowel control).
- Have poor circulation.
- Have poor feeling in your skin.
- Are not eating and drinking enough.
- Are using medication, which affects the skin for example steroids.
- Have medical devices attached to you.
Whether you are in hospital or in your own home, you will hear the following terms used as part of your care:
- Purpose T Assessment – this is an assessment to indicate your risk of developing pressure damage.
- MUST assessment – this is an assessment tool to check your nutritional status.
- SSKIN Care Plan – this is a tool used to check all 5 key areas of pressure prevention are being met.
How can I help prevent pressure damage?
In certain situations, pressure damage will still occur despite best efforts to prevent it.
The SSKIN Care Plan is used in many NHS Trusts for the purpose of pressure ulcer prevention.
It focuses on 5 important interventions:
- S – Skin – are there any signs of pressure damage or redness to the skin?
- S – Surface – is there a need for a ‘special’ mattress or cushion, if so; is it working properly and being used correctly?
- K – Keep moving – regular positional changes for those who are not active or have limited mobility. You should spend no more than 2 hours in the same position.
- I – Incontinence – regular checking of pads, toileting needs and changing as needed.
- N – Nutrition – checking you are eating and drinking well and refer to the GP for advice about diet, if needed.
You can help reduce the risk of developing a pressure ulcer by moving on a regular basis to ease the pressure on your skin and by eating a healthy balanced diet.
Your skin provides a barrier to protect you from many things including harmful substances, bacteria and infection. It is important your skin is well cared for. If you are unable to check your own skin, a nurse, relative or carer can do so with your consent.
If a medical device is in use, speak to your nurse or doctor about how to relieve pressure that may be caused by the medical device.
You must tell your nurse, relative or carer if you feel sore, numb, tingling or if your skin becomes discoloured (redness or darker areas).
What else can I do to help?
You should try to:
- Eat a healthy balanced diet and drink plenty of fluids (not alcohol).
- Keep your skin clean and well moisturised.
- Avoid using highly perfumed soap and shower gel as they can irritate your skin.
- Allow staff, relatives or carers to help you if you have difficulty changing your position.
- Remember, it is important to seek advice early from your nurse, GP, relative or carer if you notice any skin changes or tenderness of your skin.
How should your skin be cared for?
You should:
- Wash skin using a soap substitute such as Aqueous Cream or Emulsifying Ointment.
- Use warm, not hot tap water.
- Gently pat, not rub, the washed area dry with a clean towel or soft dry cloth.
Your doctor or nurse may prescribe a barrier cream such as Sorbaderm® if the skin is intact or a barrier film such as Sorbaderm® spray or foam applicator if the skin is broken, for you to apply.
You must not:
- Use soap, shower gel or foamy cleansers as these can change the natural pH of the skin.
- Use baby or wet wipes to wash or cleanse the skin.
- Use creams such as Sudocrem®, Metanium®, Drapolene® or Conotrane® as they affect the way continence pads/products work.
- Place absorbent square pads on the bed especially if using an airflow mattress as they can affect the way the mattress works.
What can I expect to happen if I am in hospital?
A nurse will assess (check) your risk of developing a pressure ulcer and may ask to inspect your skin regularly throughout your stay in hospital. How often this is done will depend on how active and well you are; everyone is different.
If you are considered at risk of developing a pressure ulcer, a plan of care will be agreed with you. All the standard mattresses used on hospital beds are made from special foam that helps reduce the risk of developing a pressure ulcer. However, for some patients a special mattress and/or cushion may be provided.
Pressure ulcers can sometimes develop even when everything is being done to prevent them, especially if you are very ill.
If you develop or have a pressure ulcer, you may need treatment to help it heal. Treatment may include dressings, removing damaged skin, use of a special mattress and/or cushion and other methods of helping your pressure ulcer to heal.
A nurse will work with you to decide the best treatment for your pressure ulcer, including the use of pressure relieving equipment.
What can I expect to happen if I am in my own home or a care home?
A nurse or carer will assess your risk of developing a pressure ulcer and may ask to inspect your skin regularly. How often this is done will depend on how active and well you are, everyone is different.
If you are considered at risk of developing a pressure ulcer, a plan of care will be agreed with you. You may be provided with a special mattress and/or cushion which will help to reduce the risk of you developing a pressure ulcer.
If you are in a residential care home setting this mattress and/or cushion will be supplied by the care home.
If you are in your own home, following the community nurse assessment, a mattress and/or cushion from the Tees Community Equipment Store (TCES) may be supplied.
As mentioned previously, pressure ulcers can sometimes develop even when everything is being done to prevent them, especially if you are very ill.
If you develop or have a pressure ulcer, you may need treatment to help it heal. If you live in a care home, you may be referred to your GP or a Community nurse for this treatment.
Treatment may include dressings, removing damaged skin, use of a special mattress and/or cushion and other methods of helping your pressure ulcer to heal. A nurse will work with you to decide the best treatment for your pressure ulcer, including the use of pressure relieving equipment.
What will happen to any photographs that are taken of my pressure ulcer?
As part of your treatment, some kind of photographic record may be made, for example clinical photographs. You will always be told if this is going to happen. The photograph will be kept as part of your healthcare record.
This means it will be seen only by those involved in providing you with care or those who need to check the quality of care you have received.
The use of photographs is very important in teaching and medical research. Because of this, your permission for use of photographs will be asked and then documented. We will not use these photographs in a way that would allow you to be identified or recognised, without your permission.
If you do not want your photographs to be used for teaching purposes please tell your doctor or nurse. If a doctor or nurse wishes to use these outside North Tees and Hartlepool NHS Foundation Trust or for publication, you will be asked to give written consent. A full explanation will be given before you are asked to sign the consent form.
Contact numbers
Single Point of Access for Community Nursing
Telephone: 01429 522500
Monday to Friday, 8.00am to 10.00pm
Weekends and Bank Holidays, 08.00am to 08.00pm
Tees Community Equipment Store (TCES)
Telephone: 01642 224205
Monday to Friday, 9.00am to 5.00pm
NHS Choices
Telephone: 111 (when it is less urgent than 999)
Calls to this number are free from landlines and mobile phones
or via the website at www.nhs.uk
Further information available
National Institute for Health and Care Excellence (NICE) Guideline, Pressure Ulcers: ‘Prevention and Management’ April 2014
www.nhs.uk/conditions/pressure-ulcers
References
- National Institute for Health and Care Excellence (NICE) Guideline Pressure Ulcers: ‘Prevention and Management’ April 2014, https://www.nice.org.uk/guidance/cg179
- National Institute for Health and Care Excellence (NICE) Quality Standard ‘Pressure Ulcers’ June 2015, https://www.nice.org.uk/guidance/qs89
Comments, concerns, compliments or complaints
Patient Experience Team (PET)
We are continually trying to improve the services we provide. We want to know what we’re doing well or if there’s anything which we can improve, that’s why the Patient Experience Team (PET) is here to help. Our Patient Experience Team is here to try to resolve your concerns as quickly as possible. The office is based on the ground floor at the University Hospital of North Tees if you wish to discuss concerns in person. If you would like to contact or request a copy of our PET leaflet, please contact:
Telephone: 01642 624719
Freephone: 0800 092 0084
Opening hours: Monday to Friday, 9:30am to 4:00pm
Email: [email protected]
Out of hours
Out of hours if you wish to speak to a senior member of Trust staff, please contact the hospital switchboard who will bleep the appropriate person.
Telephone: 01642 617617
Data protection and use of patient information
The Trust has developed Data Protection policies in accordance with Data Protection Legislation (UK General Data Protection Regulations and Data Protection Act 2018) and the Freedom of Information Act 2000. All of our staff respect these policies and confidentiality is adhered to at all times. If you require further information on how we process your information please see our Privacy Notices.
Telephone: 01642 383551
Email: [email protected]
Privacy NoticesLeaflet feedback
This leaflet has been produced in partnership with patients and carers. All patient leaflets are regularly reviewed, and any suggestions you have as to how it may be improved are extremely valuable. Please write to the Clinical Governance team, North Tees and Hartlepool NHS Foundation Trust, University Hospital of North Tees, TS19 8PE or:
Email: [email protected]
Leaflet Reference: PIL1294
Date for Review: April 2027


