Hip, Back and Pelvic pain in Pregnancy
Information for patients
This leaflet can be made available in other formats including large print, CD and Braille and in languages other than English, upon request.
This leaflet has been created to explain and provide advice on pregnancy related Pelvic Girdle Pain (PRPGP), lower back pain and/or hip pain related to your pregnancy.
In this leaflet you will find information and resources to help self-manage your PRPGP symptoms and their impact on your day to day life.
If, however, after following advice listed you are still struggling or need further advice please contact your maternity team for a referral into the physiotherapy team.
The advice in this leaflet can be used even if you’re currently not experiencing any symptoms to prevent them from occurring in the future.
Introduction
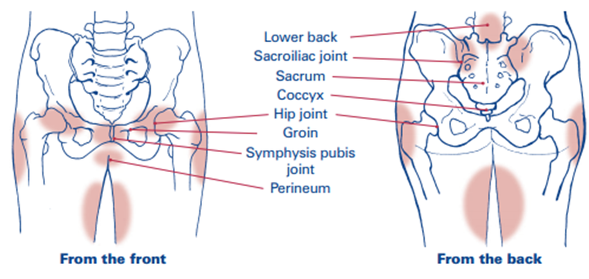
PRPGP is an umbrella team to describe pain in and around the joints that make up the pelvic girdle this includes the symphysis pubis joint (pubic bone) and/or the sacroiliac joints at the back of your pelvis, hips and lower back. This sometimes can refer down into your thighs or back of your legs.
PRPGP and lower back pain is not normal but is common in pregnancy.
Over 50% of pregnant women will experience some element of musculoskeletal pain, however the majority of them will be able to self-manage this condition.
All patients experience different symptoms and some are more severe than others.
Having symptoms does not mean that it will get worse as you progress through your pregnancy.
If you follow the advice given to manage PRPGP, it is very likely your symptoms will reduce, improve or even end.
What is the cause of PRPGP?
The exact cause of PRPGP is still not fully understood. It is likely to be a combination of factors, such as;
- The way the muscles around the pelvis and back move and work can change during pregnancy.
- Changes within the different body systems like the heart, lungs, breathing and digestive system.
- Changes in posture, or the way that you do some activities as sit to stand, walking, climbing stairs, putting extra pressure on the pelvis.
- Increased or decreased movements around the pelvis.
- Previous injury to the pelvis or hip/previous lower back pain.
What can increase the risk of PRPGP?
If you have one or more of the risks below you are more likely to experience PRPGP during pregnancy:
- Previous/ongoing lower back pain.
- PRPGP in last pregnancy.
- High demanding job and/or prolonged postures.
- Previous pregnancies.
- Increased body mass index (BMI).
- Previous injury to the pelvis.
What are the symptoms of PRPGP?
- Difficulty walking or sitting too long.
- Pain when standing on one leg (e.g. up and down stairs, in and out the bath or getting dressed).
- Difficulty moving your legs apart (e.g. getting in and out of a car or turning in bed).
- Clicking or grinding in the pelvic area.
- Difficulty laying in certain positions.
What is the treatment of PRPGP?
There are several treatments that can assist in improving and managing PRPGP symptoms. We strongly advise to follow all these tips to have optimal benefits.
The 5 Pillars: Exercise, Pelvic Health, Relaxation, Sleep Care and Pain Relief.
Exercise
Exercise is very beneficial for both mother and baby in pregnancy.
Not only does it reduce the risk of diabetes, pre-eclampsia and heart conditions. It also reduces the length of labour and has a positive effect on your baby’s heart rate, making them stronger during labour.
Other positive effects are improving fitness, stamina, sleep, mood and enhances your post-natal recovery.
Exercise in pregnancy is safe and highly recommended for you and your baby, however, if you are new to exercise, start gradually.
If you have any underlying health conditions, specifically pregnancy related, please consult a healthcare professional prior to starting exercise.
On the following page is the physical activity guidelines for pregnant patients.
It recommends that all pregnant patients should commit to 150 minutes of moderate exercise per week (i.e. 30 min a day with 2 days rest). It should include at least 2 muscle strengthening sessions e.g. yoga or Pilates.

Pelvic Health
The Pelvic Floor
The pelvic floor is a small group of muscles that support the organs within the pelvis, and aid the function of your bladder and bowel. The pelvic floor also plays a very important role in sexual function and enjoyment.
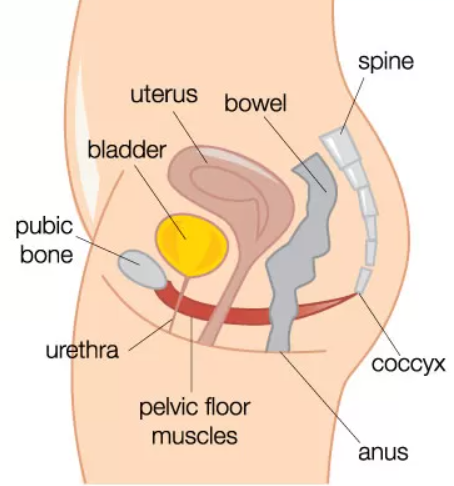
Pelvic floor exercises can have a lot of benefits in pregnancy including assisting with effective labour contractions, aids in baby positioning and helps to avoid post labour issues such as incontinence and prolapse.
It enables muscles to move through full range improving blood flow to the area promoting healthy muscle fibres and good tone.
As your body grows the pressure onto the pelvic floor increases, leading to a pelvic floor dysfunction such as leaking when you laugh, sneeze or cough. This may also cause sudden urges to need the toilet.
If you become pregnant in your late 30s or older, you are at an increased risk of developing a pelvic floor dysfunction during pregnancy, as your pelvic floor is already weakened by the drop in your oestrogen levels.
Pelvic Floor Exercises
Aim to do these 3 times a day if you are experiencing symptoms or to prevent symptoms from occurring:
- Start in a laying down position.
- Breathe in and out throughout this exercise and relax all your external muscles like your bottom and belly.
- Squeeze through your back passage – as if to stop yourself passing wind.
- Then through your vagina – as if you were to stop yourself urinating.
- Then zip up towards your belly button – like a ‘lift’ going up to a higher floor.
- Hold in this position for up to 10 seconds – you may only manage a few seconds before you start to feel the muscles quiver, but with time and practice, slowly increase this.
- Relax when your muscles quiver – letting them relax totally, like the ‘lift’ returning to ground floor.
- Relax for 10 seconds.
- Both the squeeze and the relaxing are as important.
- Report the above 10 times.
- Now do 10 fast contractions – this is the same method as above but shorter squeezes.
- Contract for 1 second and then relax for 1 second.
- Repeat this 10 times.
Optimal Toileting
Constipation is common and is suggested to affect 4 out of 10 pregnancies. As your baby grows, the womb also increases pressure applied to the bowel making it harder for bowel movements.
Constipation can improve if you follow the ‘To Do’ below:
- Eat a healthy diet including fibre (aim for 35 grams of fruit and vegetables per day).
- Exercise regularly. Improves digestion and bowel transit.
- Stay hydrated (aim for 1.5 to 2 litres per day, increase to 3 litres if warm or exercising).
- Do not strain or hold your breath on the toilet.
- Place a step stool under your feet so your knees would be above the hips creating an optimal bowel angle for movements and reducing strain.
- Do your belly breathing technique.
Relaxation
It is important to reduce any stress and allow yourself time to relax and have some ‘you time’ during pregnancy as this can help to manage any pain.
As little as 5 minutes of relaxation or belly breathing is very effective in reducing stress.
There are several types of relaxation techniques such as visualisation, breathing, meditation, mindfulness, hypnobirthing (self-hypnosis techniques to help relax the body before and during labour and birth).
The use of technology, specifically social media, has an effect on our mental health.
If you struggle to find the time to implement activities that press the pause button, like mindfulness or breathing exercises, perhaps you could try limiting your technology and social media usage.
This could be done by spending 1 or 2 days a week off technology and social media, or limiting your usage on a daily basis.
Sleep care
Sleep plays a vital role in good health and well-being throughout your life. Getting enough quality sleep at the right times can help protect your mental health, physical health, quality of life, and safety.
During pregnancy this can become increasingly difficult due to several factors which can include, baby movements, increased urine frequency at night, restless legs and heartburn.
Below are some tips to help improve your sleep:
- Reduce caffeine intake (e.g. tea, coffee, cola and chocolate).
- Have a sleep routine – use an alarm clock if needed. Going to sleep and waking at a set time allows your internal body clock to set a routine, you will find getting to sleep a lot easier. You should aim to have 7 to 9 hours of sleep per night.
- Reduce light exposure 1 hour before bed. Dim the lights an hour or so leading up to going to bed. Do not use electronic devices or watch the TV for at least 1 hour leading up to bed time and block out any light with blackout blinds or a facemask.
- Optimal bedroom conditions (cave conditions) – cool, dark and quiet. Keep the room cool; approximately 15 to 19 degrees Celsius. Using ear plus may also help.
- If you are overthinking or clock watching and unable to switch off, take a note pad to bed and write down things on your mind and deal with them in the morning. Turn the clock around, or put it somewhere you cannot see it.
- Try not to go to bed for at least an hour after you have eaten.
- Some foods increase the melatonin (sleep hormone) levels in your system, such as Kiwis. Eating 2 Kiwis, 1 hour before going to sleep may help to sleep sooner and better.
- If you wake and cannot settle. Get out of bed and sit downstairs with a dim light and read something relaxing.
- Use relaxation techniques and/or breathing techniques.
Pain Relief
Paracetamol is safe during pregnancy and may be helpful if taken regularly (1g every 4 to 6 hours).
If you need stronger pain relief, your doctor will discuss this with you.
Other ways to help manage your pain include:
- Heat: apply over tender areas like lower back, hips and buttocks for 10 to 20 minutes. You can use a hot pack or water bottle. Do not apply directly to the skin or bump.
- Ice: placing a bag of frozen peas or ice cubes in a damp tea towel and apply on the pubic joint for 5 to 10 minutes.
- Massage: Gentle massage over the lower back, thighs and buttocks may help to relieve muscular tension.
Other Musculoskeletal conditions common in pregnancy
There are other musculoskeletal conditions associated with pregnancy such as Carpal tunnel syndrome and Diastasis Rectus Abdominus (DRA).
For further advice on these please discuss with your healthcare professional – GP, Midwife, Physiotherapist or Consultant.
Further information available
- POGP (Pelvic, obstetric, gynaecological physiotherapy)
https://thepogp.co.uk/_userfiles/pages/files/POGP-PGP(Pat)(UL).pdf
- Sleep Council https://sleepcouncil.org.uk/
External Sources
- The internet supply’s several method of relaxation – audios, visual and videos – one of which may suit you better.
- Other techniques such as hypnobirthing with is largely utilised in pregnancy. Hypnobirthing is a complete birthing education guide which simply teaches you to relax with relaxation techniques and self-hypnosis. For further advice, please discuss with your midwife.
- There are several relaxation Smart Apps you can download to your devices including: Headspace, Calm and breath.
References
The Pelvic Partnership (2017) PGP National Guidelines. Accessed on 06/06/23. Available at https://pelvicpartnership.org.uk/about-pgp/
The pelvic obstetric & gynaecological physiotherapy. POGP. Accessed 01/06/23. https://thepogp.co.uk/patient_information/womens_health/pregnancy_pgp_lbp.aspx
Royal College of Obstetricians and Gynaecologists (2015) Pelvic girdle pain and pregnancy. Accessed 20/06/23:
Evidently Cochrane (2016) Easing the strain: put your feet up for constipation. Accessed 04/07/23 Easing the strain: put your feet up for constipation – Evidently Cochrane
The Sleep Council Organisation (2017) Seven Steps to get a better night’s sleep. Accessed 18/07/23. Available at: How to sleep well: 7 steps to a great night’s sleep | Age UK
Images
Pelvic floor muscles. https://www.continence.org.au/about-continence/continence-health/pelvic-floor
UK Chief medical officer (2019) Physical activity guidelines for pregnant women. Accessed 20/05/19
Comments, concerns, compliments or complaints
Patient Experience Team (PET)
We are continually trying to improve the services we provide. We want to know what we’re doing well or if there’s anything which we can improve, that’s why the Patient Experience Team (PET) is here to help. Our Patient Experience Team is here to try to resolve your concerns as quickly as possible. The office is based on the ground floor at the University Hospital of North Tees if you wish to discuss concerns in person. If you would like to contact or request a copy of our PET leaflet, please contact:
Telephone: 01642 624719
Freephone: 0800 092 0084
Opening hours: Monday to Friday, 9:30am to 4:00pm
Email: [email protected]
Out of hours
Out of hours if you wish to speak to a senior member of Trust staff, please contact the hospital switchboard who will bleep the appropriate person.
Telephone: 01642 617617
Data protection and use of patient information
The Trust has developed Data Protection policies in accordance with Data Protection Legislation (UK General Data Protection Regulations and Data Protection Act 2018) and the Freedom of Information Act 2000. All of our staff respect these policies and confidentiality is adhered to at all times. If you require further information on how we process your information please see our Privacy Notices.
Telephone: 01642 383551
Email: [email protected]
Privacy NoticesLeaflet feedback
This leaflet has been produced in partnership with patients and carers. All patient leaflets are regularly reviewed, and any suggestions you have as to how it may be improved are extremely valuable. Please write to the Clinical Governance team, North Tees and Hartlepool NHS Foundation Trust, University Hospital of North Tees, TS19 8PE or:
Email: [email protected]
Leaflet reference: PIL1468
Date for Review: December 2026
