Information for patients
This leaflet can be made available in other formats including large print, CD and Braille and in languages other than English, upon request.
What is oesophageal manometry?
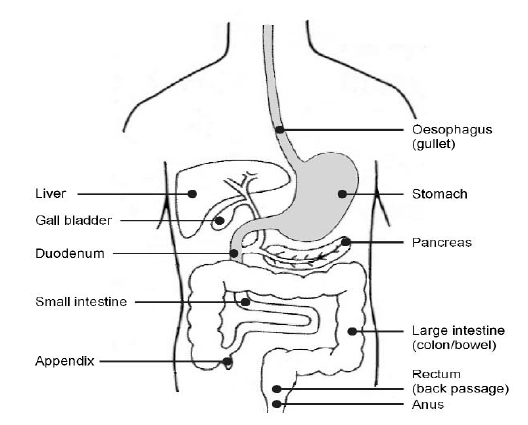
This is a procedure which measures the pressure inside your oesophagus (gullet) using a manometer (a tube which measures the pressure of a liquid or a gas). It shows whether your oesophagus is working correctly or not. It can also show if your symptoms are due to a disorder or a problem with your oesophagus.
The procedure is also used before an operation for anti-reflux (the back flowing of liquid or acid). This is to make sure your oesophagus is working well enough for you to have your operation.
Why do I need a manometry?
This procedure is done prior to fundoplication surgery.
This is generally key hole surgery and involves wrapping a part of the stomach around the lower end of your food pipe to prevent acid welling up into the oesophagus. Manometry is used to make sure your food pipe is working normally and adequately prior to under taking the operation.
Sometimes, the oesophagus (gullet) may not work or be working effectively, causing problems with swallowing and keeping food and fluids down. This test will diagnose the problem of how the oesophagus works.
What are the possible side effects, risks or complications?
The common side effects of this procedure include:
- runny nose (while the tube is being inserted)
- local bleeding (this usually stops quickly, but you must tell the nurse/doctor if you are using blood thinning medication (such as aspirin) and any previous surgery to the nose
- medical spray used to numb the nose and throat may cause a stinging sensation, but this should quickly wear off.
- sore throat (up to 24 hours)
- slight discomfort on swallowing (which will stop once the test is over).
Very occasionally some patients may feel faint during the procedure. There is also a very small risk of this procedure causing other complications such as bleeding from damage or perforation to:
- the inside of your nose
- your throat
- your larynx (voice box)
- your oesophagus
- your stomach.
Passing the tube is done without sedation as full cooperation from is required during the procedure.
This is not a comfortable procedure, however it is generally well tolerated if you follow the instructions clearly and keep calm and composed.
The entire procedure will take approximately 40 minutes.
Careful monitoring (checking) by your doctor or specialist nurse will make sure any problems are identified and treated quickly.
What should I do before my procedure?
7 days before your procedure you must stop taking any anti-emetic (anti-sickness) medications such as metoclopramide (Maxolon), prochlorperazine (Stemetil), ondansetron (Zofran) or domperidone (Motilium).
You should continue to take any PPI medication, such as Lansoprazole, Omeprazole and Esomeprazole.
If you have diabetes you should contact your diabetic liaison nurse for advice. (See contact numbers)
On the day of your procedure you must:
- not eat anything for 4 hours before the time of your appointment
- not drink any fluids for 2 hours before the time of your appointment
- continue to take all your normal medication except any anti-emetics
- wear comfortable, loose clothing.
What will happen when I arrive at the hospital?
Your appointment letter will tell you when and where to go for your procedure. The procedure takes about 40 minutes but please note we operate a ‘list system’. This means you will be seen when it is your turn and not the time given for you to arrive at the unit.
When you arrive at the unit your doctor or specialist nurse will make sure you understand what is involved in the procedure and will answer any questions you may have. Once you understand the procedure and have agreed to go ahead, you will be asked to sign a consent form.
What will happen during the procedure?
Your doctor or specialist nurse will make sure you are comfortable. You will be asked to sit upright and some local anaesthetic spray will be sprayed inside your nose to numb the area.
Your doctor or specialist nurse will then pass a thin plastic tube up the inside of your nose. This tube will pass through your nose and down your throat until it reaches your stomach.
To help the tube pass smoothly through your nose and throat you may be asked to sip and swallow some water, adding to the reason why sedation cannot be given for this procedure.
Once the tube is in place inside your stomach you will be asked to lie flat. You will be aware of the tube in the back of your throat and this may feel a little uncomfortable.
The tube is connected to special equipment which allows the pressure inside your oesophagus to be measured and shown as a graph on a computer screen. This can take up to 20 – 30 minutes.
During the procedure a nurse will continue to give you small, measured amounts of water, so the doctor and specialist nurse can check the muscle contractions in your oesophagus as you swallow the water.
This may be repeated up to 20 times and is sometimes called “wet swallows”. You may also be asked to chew and swallow some bread or biscuits.
What will happen after the procedure?
When the procedure is completed the tube will be removed and you will be allowed to go home. You can usually eat and drink and take your medication as normal, after the procedure. You may need to have another procedure called a 24-hour pH monitoring study. If this is needed, you will usually be given an appointment before you leave the unit.
If available, your doctor or specialist nurse will have discussed this procedure with you and will give you a leaflet, ’24-hour pH monitoring study’. If you have an urgent problem the night after your oesophageal manometry, you should contact your local Accident and Emergency Department.
When will I know the results from the procedure?
The results will be sent to the consultant in charge of your care who referred you for this procedure and who will discuss these with you at your next outpatient appointment.
Contact numbers
If you need further advice, or have any problems, please contact the appropriate number below:
University Hospital of Hartlepool
Rutherford Morison Unit
Telephone: 01429 522356
Monday – Friday, 8.00am – 6.30pm
Diabetes Liaison Nurses
Telephone: 01429 522594
Monday – Friday, 9.00am – 5.00pm
Accident and Emergency Department
Telephone: 01642 382899
24 hours a day, 7 days a week
If you have any worries or concerns, you should contact your GP during normal surgery hours. Outside surgery hours, you should contact your GP’s surgery for the Out of Hours Service number.
Further information is available from:
NHS Choices
Telephone: 111 (when it is less urgent than 999)
Calls to this number are free from landlines and mobile phones.
or via the website at www.nhs.uk
Information used in the development of this leaflet
Bodger K & Trudgill N (2006) Guidelines for Oesophageal Manometry and pH Monitoring, British Society of Gastroenterology.
Comments, concerns, compliments or complaints
Patient Experience Team (PET)
We are continually trying to improve the services we provide. We want to know what we’re doing well or if there’s anything which we can improve, that’s why the Patient Experience Team (PET) is here to help. Our Patient Experience Team is here to try to resolve your concerns as quickly as possible. The office is based on the ground floor at the University Hospital of North Tees if you wish to discuss concerns in person. If you would like to contact or request a copy of our PET leaflet, please contact:
Telephone: 01642 624719
Freephone: 0800 092 0084
Opening hours: Monday to Friday, 9:30am to 4:00pm
Email: [email protected]
Out of hours
Out of hours if you wish to speak to a senior member of Trust staff, please contact the hospital switchboard who will bleep the appropriate person.
Telephone: 01642 617617
Data protection and use of patient information
The Trust has developed Data Protection policies in accordance with Data Protection Legislation (UK General Data Protection Regulations and Data Protection Act 2018) and the Freedom of Information Act 2000. All of our staff respect these policies and confidentiality is adhered to at all times. If you require further information on how we process your information please see our Privacy Notices.
Telephone: 01642 383551
Email: [email protected]
Privacy NoticesLeaflet feedback
This leaflet has been produced in partnership with patients and carers. All patient leaflets are regularly reviewed, and any suggestions you have as to how it may be improved are extremely valuable. Please write to the Clinical Governance team, North Tees and Hartlepool NHS Foundation Trust, University Hospital of North Tees, TS19 8PE or:
Email: [email protected]
Leaflet reference: PIL1242
Date for review: 18/09/2023
