Information for patients
This leaflet can be made available in other formats including large print, CD and Braille and in languages other than English, upon request.
A nuclear medicine test involves giving you a small amount of a radioactive dye. We can then see where this goes in the body or how your body processes it. Each nuclear medicine test is performed for a specific purpose.
This leaflet will explain the potential risks from the small amounts of radioactive substances used in nuclear medicine tests. It does not apply to other kinds of imaging such as ultrasound and MRI imaging.
Why am I having a nuclear medicine test?
Nuclear medicine tests have many uses including:
- To help find out what is wrong with you
- To check on progress of an illness or injury
- to help determine chemotherapy drug dosage
- to help carry out surgery as part of your diagnosis/treatment
- to provide your doctor with other clinical information
The healthcare professionals involved in your test always check that the benefit of having the test is greater than the risk from the small amount of radioactive substance given.
Nuclear medicine tests use a small amount of radioactive substance to see how your body works. You will be radioactive for a short while after your test – normally just for 1 day. Radioactive substances like X-rays are capable of causing a process known as ionisation.
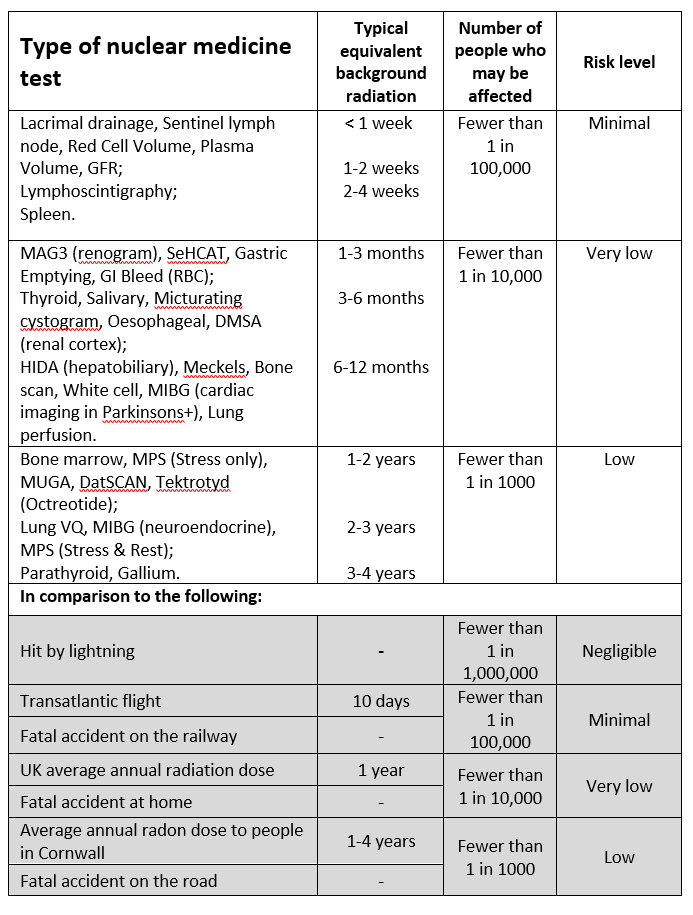
Nuclear medicine covers a large range of studies. The table below lists many of the tests we perform. Your healthcare team should tell you which test they would like you to have.
Are there any risks in using ionising radiation?
We are all exposed to background radiation every day. Any amount of radiation has potential ill health effects (very small increased chance of cancer).
We are all at risk of developing cancer during our lifetime. The normal risk is that this will happen to about 50% of people at some point in their life (1 in 2).
The table below tells you how much radiation you are likely to get from different types of nuclear medicine tests, compared to other every day activities, and how this may affect your cancer risk.
Further risk comparisons can be found at: https://www.gov.uk/government/publications/ionising-radiation-dose-comparisons/ionising-radiation-dose-comparisons
What if I may be pregnant or if I am chest/breastfeeding?
You should tell your healthcare team if there is any possibility of being pregnant or if you are chest/breastfeeding.
Exposure of an unborn baby to ionising radiation may cause a slight increase in the cancer risk to them. Nuclear medicine tests are often avoided in pregnancy, unless the risk of not performing the test is greater.
Our radioactive dyes can be expressed in human milk. The nuclear medicine team will give you advice on how to reduce the risk to a chest/breastfeeding baby. You may be advised to discard the milk that you produce and swap to a suitable formula for a short period of time.
What about children?
Younger people have a slightly increased risk from exposure to ionising radiation and radioactive materials. The healthcare team take account of this when deciding if a child needs a nuclear medicine test, and the amount of radioactivity used is kept as low as possible.
What if I don’t have the test?
The risk of not having the test is that it may not be possible to find out what is wrong with you, or how best to treat you. You should discuss any concerns with your healthcare team.
What if I have more questions?
Please talk to your doctor or any of the team carrying out your nuclear medicine test if you would like to discuss any of this further.
Information produced by:
Northern Medical Physics & Clinical Engineering,
North Tees & Hartlepool NHS Foundation Trust
July 2023.
References
- Notes for guidance on the clinical administration of radiopharmaceuticals and use of sealed radioactive sources, Administration of Radioactive Substances Advisory Committee (2023).
2. Radiation Risk from Medical X-ray Examinations as a Function of the Age and Sex of the Patient (HPA-CRCE-028), Health Protection Agency (2011).
3. Ionising Radiation Exposure of the UK Population: 2010 Review (PHE-CRCE-0.26), Public Health England (2010)
Further Reading
Comments, concerns, compliments or complaints
Patient Experience Team (PET)
We are continually trying to improve the services we provide. We want to know what we’re doing well or if there’s anything which we can improve, that’s why the Patient Experience Team (PET) is here to help. Our Patient Experience Team is here to try to resolve your concerns as quickly as possible. The office is based on the ground floor at the University Hospital of North Tees if you wish to discuss concerns in person. If you would like to contact or request a copy of our PET leaflet, please contact:
Telephone: 01642 624719
Freephone: 0800 092 0084
Opening hours: Monday to Friday, 9:30am to 4:00pm
Email: [email protected]
Out of hours
Out of hours if you wish to speak to a senior member of Trust staff, please contact the hospital switchboard who will bleep the appropriate person.
Telephone: 01642 617617
Data protection and use of patient information
The Trust has developed Data Protection policies in accordance with Data Protection Legislation (UK General Data Protection Regulations and Data Protection Act 2018) and the Freedom of Information Act 2000. All of our staff respect these policies and confidentiality is adhered to at all times. If you require further information on how we process your information please see our Privacy Notices.
Telephone: 01642 383551
Email: [email protected]
Privacy NoticesLeaflet feedback
This leaflet has been produced in partnership with patients and carers. All patient leaflets are regularly reviewed, and any suggestions you have as to how it may be improved are extremely valuable. Please write to the Clinical Governance team, North Tees and Hartlepool NHS Foundation Trust, University Hospital of North Tees, TS19 8PE or:
Email: [email protected]
Leaflet reference: PIL1451
Date for Review: September 2026
