Information for patients
This leaflet can be made available in other formats including large print, CD and Braille and in languages other than English, upon request.
Introduction
This leaflet is for patients to explain what an Indwelling Pleural Catheter (IPC) is, why it may be useful and how it is inserted.
What is an Indwelling Pleural Catheter?
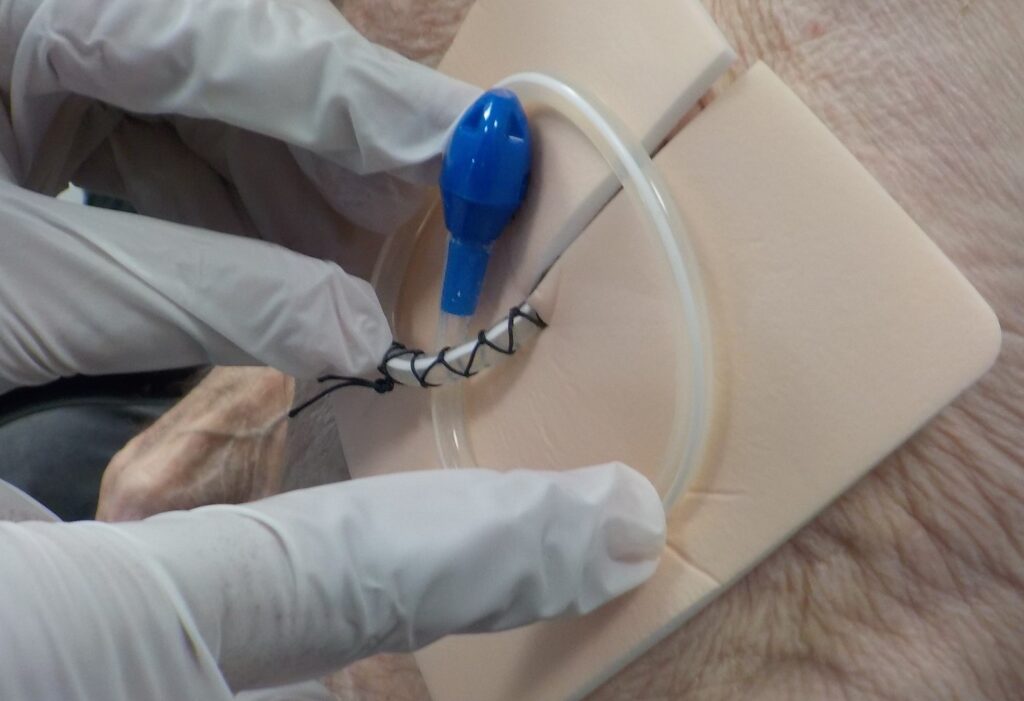
It is a small tube to drain fluid off from the space between the lung and the inside of the chest wall, easily and painlessly whenever it is needed. The tube is soft, flexible and thinner than a pencil. It remains inside the chest and passes out through the skin.
When fluid needs to be removed, a special bottle is attached to the tube and fluid is drained out.
What is the benefit of an Indwelling Pleural Catheter?
When you take a breath in, your lung follows the inside of your rib cage as it moves, but they are not stuck together. There is a double layered covering (the pleura), rather like (cling film), between the outer surface of the lungs and the inside of the rib cage. It is lubricated and allows the lungs to move with the rib cage when you breathe in and out. In your case, fluid has built up between these layers and this is limiting how much your lung can expand. This may be making you breathless. In your case, there is a high chance the fluid will continue to accumulate even if we take out the fluid that is currently there.
Placing an Indwelling Pleural Catheter allows fluid to be drained whenever required to improve your breathing .This can be done by a nurse, or you and/or your relative can be trained to do this.
What are the risk of an Indwelling Pleural Catheter?
Inserting a catheter is a routine and safe procedure performed in the outpatients department.
There are potential risks which your doctor will explain:
- Pain/Discomfort – Most people get some discomfort from their catheter in the first week. We will ensure you have pain killing medication to control this.
- Infection – This is uncommon (5 in 100 patients 1, 2). There will be full instructions on how you and your nurses can reduce the risk of infection, and what warning signs of infection to look for. Minor infections where the tube goes through the skin can be easily treated with antibiotic tablets. More Deep-seated infection may need antibiotic injections and very occasionally admission and removal of the catheter.
- Bleeding – Very rarely, (less than 1 in 100 patients 1) a blood vessel can be damaged during insertion which causes significant bleeding needing an operation to stop this. Our team is very experienced and try their best to avoid this.
- Tube Blockage – Sometimes the catheter can become blocked due to the disease in your chest .If this happens, we may be able to unblock using medication put through the catheter.
- Chest Wall – Very rarely, if cancer is present, it can spread along the site of the catheter causing lumps under the skin.
When is an Indwelling Pleural Catheter removed?
They are designed to remain in position permanently. However if it becomes blocked or the fluid dries up, it can be removed.
Preparing for the procedure
- Before the procedure – Your doctor will arrange for some simple blood tests to make sure you are not at high risk of bleeding. If you are on blood thinning medications (e.g. wafarin, tinzaparin, enoxaparin, rivaroxaban or apixiban) you will be given specific instructions which may involve stopping the medications; if you are unclear about this please contact the team.
- On the day of the procedure – You can drive yourself although it is often best to have someone bring you and stay with you whilst you are in the clinic. You can eat and drink as normal for this procedure and you should take all your usual medications unless specially instructed by the team.
- On the day of the procedure – You can drive yourself although it is often best to have someone bring you and stay with you whilst you are in the clinic. You can eat and drink as normal for this procedure and you should take all your usual medications unless specially instructed by the team.
How is the procedure performed?
The doctor performing the procedure will explain the whole procedure to you and ask you to sign a consent form. After this, the team will place you in a comfortable position allowing the doctor to access your chest – typically by asking to lie on your side or a couch.
The procedure takes about 30 minutes and is performed by:
- The doctor will use a jelly scan (Ultrasound) to find the best place to get the fluid.
2. The doctor will then clean the site to kill any bacteria on your skin with an alcohol gel, which may feel cold.
3. The doctor will then numb the area by injecting local anaesthetic to the skin and into the chest wall.
4. Once the area is numb, the doctor will then make the two small cuts in the numb areas of the skin to create a path for the tube. This should not be painful although you may feel some pressure or tugging. One cut is for the catheter to pass through your skin, and the second is for it to be passed into the chest. The catheter is then gently positioned into the chest.

5. Once the catheter is in place, a stitch is placed at both skin cuts with one holding the catheter in place. The doctor will then drain some fluid off through the catheter.
What happens after the procedure?
The nursing staff in Lung Health are very experienced and will look after you for the next hour. If you feel unwell in anyway, please let the team know. You will have a chest X-ray and your vital signs will be checked.
Before you leave, our team will ensure you know when your first drainage will be and who will do it for you – typically this is performed by the District Nursing Team in your home after a couple of days.

After Care Advice
If you develop pain which is not responding to standard painkillers or you develop increasing breathlessness in the hours after the procedure, you should contact the Lung Clinic (9am – 5pm, Monday to Friday), or out of hours medical care (GP 111 service, or emergency services if you are feeling very unwell).
The frequency that pleural fluid is drained through the catheter varies from person to person; this starts at 2 -3 times a week, but often becomes less frequent later. Usually this is performed by a nurse attending your home, but you or a relative can be trained to perform this.
You will be taught how to clean and maintain your tube, but please ask for extra help if you remain unsure.
Providing the catheter site remains clean and dry with a dressing covering it, you will be able to bath and shower normally. After a month, it is even possible to go swimming.
If you have chemotherapy planned for cancer, placement of a pleural catheter will not affect this.
Contact Numbers
Lung Health
Monday to Friday
09:00 am – 05:00 pm
Telephone No: 01642 624 270
Department of Respiratory Medicine
Monday to Friday
09:00 am – 05:00 pm
Telephone No: 01642 624 936
References
- Lui MMS, Thomas R, Lee YCG – Complications of Indwelling Pleural Catheter use and their Management. BMJ Open Respiratory Research 2016; 3:e000123.doi: 10.1136/b,kresp-2015-000123
2. Fysh E. et al. Clinical Outcomes of Indwelling Pleural Catheter – Related Infections: An international multicentre study. Chest Vol.144 Nov 2013. Page 1597 -1602
Comments, concerns, compliments or complaints
Patient Experience Team (PET)
We are continually trying to improve the services we provide. We want to know what we’re doing well or if there’s anything which we can improve, that’s why the Patient Experience Team (PET) is here to help. Our Patient Experience Team is here to try to resolve your concerns as quickly as possible. The office is based on the ground floor at the University Hospital of North Tees if you wish to discuss concerns in person. If you would like to contact or request a copy of our PET leaflet, please contact:
Telephone: 01642 624719
Freephone: 0800 092 0084
Opening hours: Monday to Friday, 9:30am to 4:00pm
Email: [email protected]
Out of hours
Out of hours if you wish to speak to a senior member of Trust staff, please contact the hospital switchboard who will bleep the appropriate person.
Telephone: 01642 617617
Data protection and use of patient information
The Trust has developed Data Protection policies in accordance with Data Protection Legislation (UK General Data Protection Regulations and Data Protection Act 2018) and the Freedom of Information Act 2000. All of our staff respect these policies and confidentiality is adhered to at all times. If you require further information on how we process your information please see our Privacy Notices.
Telephone: 01642 383551
Email: [email protected]
Privacy NoticesLeaflet feedback
This leaflet has been produced in partnership with patients and carers. All patient leaflets are regularly reviewed, and any suggestions you have as to how it may be improved are extremely valuable. Please write to the Clinical Governance team, North Tees and Hartlepool NHS Foundation Trust, University Hospital of North Tees, TS19 8PE or:
Email: [email protected]
Leaflet reference: PIL1047
Date for Review: August 2026
