Information for patients
This leaflet can be made available in other formats including large print, CD and Braille and in languages other than English, upon request.
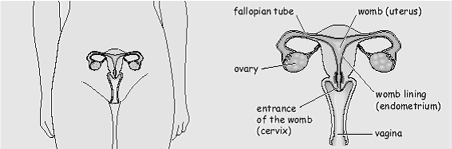
Your doctor has advised you to have a hysterectomy, this involves removal of your uterus (womb) and/or a salpingo-oophorectomy (removal of one or both of your tubes and ovaries).
What is a hysterectomy?
Hysterectomy is the name of the operation to remove your uterus with the cervix (womb and neck of the womb).
There are 3 main ways of carrying out this operation:
- abdominal hysterectomy. This means an incision (cut) is made in your abdomen (tummy).
- vaginal hysterectomy. This means an incision is made inside your vagina and there will be no visible scar.
- laparoscopically assisted vaginal hysterectomy. This means small incisions are made in your abdomen allowing the use of a camera to help remove the ovaries and tubes as well as the womb.
This is commonly referred to as “key-hole surgery”. Not all of the surgeons in the Trust offer this type of surgery and it is not suitable for everyone so you may not be offered it.
Why would I need a hysterectomy?
A hysterectomy can be advised if you have:
- heavy or irregular menstrual periods1
- a prolapse (dropping down of your womb)
- fibroids (a non-cancerous tumour or growth in your uterus)
- pelvic scar tissue caused by infection or previous surgery
- cancer of the womb, ovaries or fallopian tubes endometriosis (tissue usually found in the uterus is found elsewhere in the body, for example, fallopian tubes or ovaries).
What are the different types of hysterectomy?
There are 4 kinds of hysterectomy. The choice of operation depends on many factors. Your doctor will discuss with you the most appropriate operation for you, and why. Once you have made your decision, you will be asked to sign a consent form.
- Total hysterectomy. Your womb and cervix (neck of the womb) are removed, but your ovaries and fallopian tubes are left in place.
- Total hysterectomy and bilateral salpingo-oophorectomy. Your ovaries and fallopian tubes are removed, as well as your womb and cervix.
- Sub-total hysterectomy. Your womb is removed, but your cervix is left in place. If you have this kind of operation, you will still need to have Cervical Cancer Screening (a smear) tests.
- Wertheim or Radical hysterectomy. Your uterus, cervix, part of your vagina, parametrium (the broad band of tissue around the uterus), omentum (part of the peritoneum which lines the organs in your abdomen), lymph glands and also the fatty tissue of the pelvis are removed.
This type of hysterectomy is done for cancer and usually in a cancer centre such as James Cook University Hospital.
Are there any risks or possible complications with having a hysterectomy?
2 women in every 100 having an abdominal hysterectomy will experience at least 1 of these complications.2
- accidental injury to the bladder and/or the ureter (the tube that joins the kidney to the bladder). This can happen to 7 women in every 1,000. If this happens another operation may be needed.2
- long-term disturbance to the bladder function.2
- accidental injury to the bowel. This can happen to 4 women in every 10,000. If this happens another operation may be needed.2
- blood transfusion. 23 women in every 1,000 can suffer from heavy blood loss. If this happens, a blood transfusion may be needed.2
- return to theatre. 7 women in every 1,000, may need to go back to theatre.2
- pelvic abscess or infection. This can develop in 2 women in every 1,000.2
- death. There is a risk of death within 6 weeks. This can happen to 32 women in every 100,000.2
- risks linked with anaesthetic.2 You will be given a leaflet ‘You and your anaesthetic’ which explains in detail about anaesthesia. Your anaesthetist (a doctor with special training in anaesthetics), will discuss this with you. You may need to be admitted to the Critical Care Unit.
- deep vein thrombosis – DVT (blood clots in the leg veins) or pulmonary embolism – PE (blood clots in the lungs). This can happen to 4 women in every 1,000 having a hysterectomy.2
Some patients may develop a DVT after an operation. This can be due to the effects of the anaesthetic, bed rest and reduced activity during your recovery. Your doctor will discuss your individual risks with you.
The risk of a DVT can be reduced by slightly thinning your blood.
Before and after your operation you may be given:
- an injection into your abdomen (tummy) every night during your stay in hospital. You may notice some bruising around the injection site. This is quite normal and will disappear once the injections stop.
- a mechanical pump. This involves applying either a special slipper to each foot or a special cuff around your calf. This inflates (blows up) every so often and squeezes the veins in your foot or leg to help pump blood around your body.
- special elastic stockings or socks until you are fully mobile. If your doctor advises that you should wear these special stockings, you will be fitted with them before your operation. You will need to wear them during the day and night for 6 weeks after your operation.
You may be offered one or more of the above. It is very important that you follow the advice given by your doctor, nurse and physiotherapist to try to prevent a Deep Vein Thrombosis (DVT) developing. DVT can lead to the more serious complication of Pulmonary Embolism (PE).
Frequent risks are usually mild, but can include:2
- wound infection or bruising
- numbness, tingling or burning sensation on the wound area which can take a few months to settle
- frequency of micturition (passing urine) or urine infection
- slow wound healing
- keloid formation (thickened scar)
- early menopause
Other issues you may wish to discuss with your doctor:
- some symptoms, such as pain may continue after your operation
- need for bladder catheter and wound drain postoperatively (usually for 1 – 2 days)
- possible scar discomfort, disfigurement or hernia
- Hormone Replacement Therapy (if ovaries are removed in pre-menopausal women). Your doctor will discuss this with you.
- may affect sexual function/response in women
- may affect bowel/bladder function
- may increase the risk of development of prolapse in later life.
What does a hysterectomy mean for my future health?
- You will have no more menstrual periods.
- You will be unable to have any further pregnancies.
- You may, or may not, need to continue having cervical smears. Please check with your doctor.
If you had pelvic pain before your hysterectomy, the operation may not cure the pain completely. Your doctor will discuss this with you. If your ovaries are not removed, pre-menstrual symptoms will still occur up until the time of your menopause (change of life). This will happen earlier than expected if both of your ovaries are removed. You will experience menopausal symptoms and may need Hormone Replacement Therapy (HRT), but only if you have not had the menopause yet. If you are already taking HRT, it may need to be changed.
Will I need Hormone Replacement Therapy (HRT)?
HRT helps to prevent symptoms linked with the menopause, and is also believed to help protect women against osteoporosis (thinning of the bones) in later life.
If your doctor feels you need HRT, he or she will discuss this with you.
HRT comes in several forms; patches, tablets, gel and nasal sprays. It is usually continued until you are 50 – 51 years old, and then reviewed.
While taking HRT, you should have your blood pressure checked and have a breast examination every year. A separate leaflet is available for HRT, please ask for one if you wish to know more.
What will happen at the pre-admission clinic?
You will be asked about your general health. Your blood pressure, pulse, weight and urine will be checked. Please remember to bring a fresh sample of your urine with you and all tablets, medicines, inhalers and creams you are using.
Your nurse will tell you if you need to stop taking any of these before your operation. Samples of your blood will be taken and you may be sent for an x-ray and ECG (a heart tracing).
How can I prepare for my operation?
Before any operation, it helps to try and get as fit as possible, as this will help in your recovery. If you are overweight or smoke, seek advice from your GP who will offer you support and dietary or stop smoking advice. (See contact numbers at the end of this leaflet).
This will help reduce the risk of any complications during your anaesthetic and operation.
What I need to bring with me?
The National Institute for Health and Care Excellence (NICE) recommends you keep warm before, during and after your operation because it can reduce side effects, complications and help you recover from your operation faster.3
Please make sure you bring socks and slippers, a dressing gown, a vest or other warm clothing to help you feel warm while you are in hospital.
You should also bring any medication you are taking into hospital with you.
What will happen while I am in hospital?
On admission to the ward, you will be introduced to your ‘named nurse’ who is responsible for planning your nursing care with you. Your named nurse is part of a team of nurses who are there to help and advise you on a day-to-day basis, and to make your stay as comfortable as possible.
Hysterectomy is normally performed under either a:
- General anaesthetic – A state of carefully controlled and supervised unconsciousness that means you are unable to feel any pain.
- Spinal anaesthetic – You are awake but have an injection in your back that numbs the lower part of your body.
You will be given leaflets explaining the different types of anaesthetic. Your anaesthetist will discuss them with you when he or she visits you before your operation and advise which is most suitable for you.
What will happen before my operation?
You will be asked to remove any jewellery you are wearing (except your wedding ring), contact lenses, make-up and nail varnish and also not to use body lotions, deodorants and perfumes. You will be asked to put on a theatre gown.
False teeth and hearing aids may be removed in the operating theatre.
You may be given a ‘pre-med’ (some tablets to help you relax).
Just before the time of your operation, one of your nurses from the ward will go with you and transfer your care to a theatre nurse.
If you have any worries or concerns, tell the staff, they are there to help and support you.
Your theatre nurse will check your details again before taking you into the anaesthetic room. In the anaesthetic room, you will meet your anaesthetist again. He or she will give you your anaesthetic before you are taken into the operating theatre and will stay with you throughout your operation.
Your nurse will take your temperature before you are taken to the operating theatre. If it is below 36°C (96.8°F), the operation will not start until you are warm. A warm air blanket or jacket may be used to raise your temperature.
When in the operating theatre and the recovery room, your nurse will take your temperature regularly. If it falls below 36°C (96.8°F), you will be placed under a warm air blanket or jacket.
Please tell your nurse or doctor if you feel cold during your stay in hospital.
Before and during your operation:
- a cannula (fine needle) will be placed in the back of your hand or arm so we can inject drugs. Sometimes when drugs are injected, they may feel cold and sting a little.
- an intravenous drip may be attached to your cannula, but this usually takes place when you are asleep.
- you may be asked to breathe some oxygen through a face mask before you are given the anaesthetic.
- your blood pressure will be measured.
- your pulse will be taken, and the amount of oxygen in your blood will be measured by attaching a special clip on to your finger. This does not hurt.
- Your heart rate will be monitored by placing sticky pads on your chest. These are attached to some leads to show a tracing of your heart on a monitor. This is routine and is nothing to worry about.
Why am I asked not to eat or drink before my operation?
You must not eat or drink anything for at least 6 hours before your operation. This is very important. You must follow the instructions. Nothing means nothing at all. If you forget and do eat or drink anything then please tell your doctor or nurse, as your operation may need to be postponed for your safety.
This is because when you are unconscious, if your stomach contains food or drink you may be sick, it could get into your lungs, affect your breathing and cause an infection. Your nurse will discuss this with you.
What will happen during my operation?
You will have a drip in your arm through which you will receive fluids until you are drinking again. You will also receive antibiotics through this drip to help prevent infection. This is usually removed two days following the operation.
You may have a catheter (thin tube) which empties your bladder, and this will usually be removed on the first or second day after your operation, or when your doctor advises.
You may also have a drain in your wound, and this will be removed on the instructions of your doctor, as will your stitches or clips.
What will happen after my operation?
You may be away from the ward for several hours. At the end of your operation you will wake up in the recovery room near the operating theatre.
Specially trained nursing staff will look after you in the recovery room until you are ready to return to your ward. Many people do not remember waking up in the recovery room or returning to their ward.
Your nurse will check your blood pressure, pulse, temperature and level of pain regularly. You may continue to have oxygen through a face mask for as long as you need it to keep the oxygen in your body at the right level.
You should be able to eat and drink soon after your operation. As soon as you are able to eat and drink your drip will be removed.
You will be encouraged to get out of bed as soon as possible after your operation. This helps reduce the risks of chest infection, blood clots in your legs and the discomfort caused by ‘wind’.
Will I be in pain after my operation?
After all operations, some discomfort, soreness, or pain is to be expected, so good pain relief is important. It helps you to feel better and makes it easier to move around, take deep breaths and cough. This reduces the risk of any complications happening after surgery.
You will be offered pain relief in one or more of the following ways:
- Patient Controlled Analgesia (PCA). You can give your own pain relief, when you need it, by pressing a button attached to a machine.
- injections into your buttock (bottom) or leg.
- painkilling suppositories into your rectum (back passage).
- tablets when you are able to drink again.
When can I go home?
You will need to stay in hospital for about 1 – 5 days. This could be longer, depending on your progress. Most ladies are home by the 3rd post-operative day.
While you may feel quite well in hospital, when you go home you will feel more tired than you expected.
Try to make arrangements for extra help in your home for the first 1 – 2 weeks or longer after leaving hospital.
What problems could I have during my recovery?
While your recovery from the hysterectomy will hopefully be uneventful, some problems can happen. Most only last for a short time and a full recovery can be expected.
The most common problems are:
Vaginal discharge
A slight vaginal discharge (changing from red to pink to brown to a whitish colour) or spotting can last for up to 6 weeks after your operation.
This is normal. Sometimes, however, vaginal infections can develop because the body is not as resistant to infections immediately after an operation.
If you notice the discharge becomes redder, heavier, or offensive (smelly), then you should contact your GP. It is not uncommon for women to pass old, dark brown, blood vaginally for several weeks after surgery and this can sometimes come out as one “lump” which can be a bit worrying if you aren’t expecting it.
Urinary infection
After your operation, you may have some stinging when you pass urine, but this will soon pass. If you later develop pain or burning when passing urine, or feel that you have to go more often and only pass small amounts, then you may have an infection and should contact your GP.
Wound discomfort
At first you will have some numbness and discomfort from your wound site, particularly if you twist your body suddenly, when you will feel a pull or sharp stab.
This is quite normal and will settle in time as your wound heals.
If the area around your wound becomes reddened, hot and painful to touch, or the wound leaks any fluid, you should contact your GP for advice.
Aches and pains
General aches and pains, especially backache, are quite common after a major operation. These should gradually improve over the first few weeks.
Sleep disturbance
After you have gone home, you may be tired but find it hard to get to sleep. This may be partly due to having your routine upset while in hospital and should settle. Try reading a book and having a warm drink, then try to relax each part of your body in turn (this relieves tense abdominal muscles which may be causing discomfort).
If you continue to find it difficult to sleep, you should see your GP. It will also help if you reduce your caffeine intake (tea, coffee, chocolate, cola etc.).
Tearfulness
It is quite common to find yourself feeling weepy and low at times after the operation. This can be due to frustration at not being able to do the things you want to do.
This may happen while you are in hospital and for a couple of months after you go home, but should improve as you begin to feel better and stronger.
How long will my recovery take?
Women recover at their own rate, so do not judge yourself against other women. Usually by 6 weeks, you are feeling better and able to manage most tasks. Recovery is usually quicker after vaginal surgery.
However, complete recovery, when you are feeling fully back to normal, may take several months.
How can I help my recovery when I go home?
You may bathe or shower daily. Do not use bubble bath, as this may cause irritation.
Your diet is important, as it helps your wound to heal. Protein and Vitamin C in particular are necessary. These are found in cheese, milk, meat, fish, eggs, vegetables and fruit. Also, the dietary fibre in cereals, fruit and vegetables, helps prevent constipation, which can occur after an operation.
You should try to drink at least 1 litre (2 pints) of fluid a day.
Some exercise is important because it improves your muscle tone and blood circulation. You should wear your anti-thrombotic stockings to help reduce the risk of clots.
Some points to remember are:
- try not to put any strain on your operation site for at least 6 weeks to give your internal tissues time to heal. This means taking care when stretching or lifting.
- if you become tired, stop what you are doing and leave it for a few days before trying again.
- try not to stand still in one place for long periods of time, as this can make you feel faint.
- walking is a very good exercise. You should start with a 10 minute walk every day, increasing the length as you feel able. You may walk up and down the stairs straight away.
- you may start swimming and do activities such as light gardening from 4 – 6 weeks after your operation. Heavy spadework and strenuous activities such as cycling and aerobics should be left for 3 months.
- you should not drive for 3 – 4 weeks as you may have difficulty concentrating. You may also find it uncomfortable to do an emergency stop. Please check with your car insurance company.
- you should do your pelvic floor exercises which will be explained to you.
When can I resume sexual intercourse?
Sexual activity can usually be re-started about 4 – 6 weeks after your operation. This allows time for healing to take place. Intercourse may be a little uncomfortable at first, or feel different. If your partner is gentle and you use a lubricating jelly, this should help.
When can I return to work?
This can vary from 4 – 12 weeks after your operation, depending on the type of work you do and what the operation was for. Ask your GP when the time is right for you.
Will I need a follow-up appointment?
An appointment letter for about 6 weeks after your operation will be sent to you through the post, if needed. Your nurse will discuss this with you.
Old wives’ tales
You may have heard stories that having a hysterectomy results in some undesirable side-affects. It has been claimed this operation leads to early ageing, growth of facial hair, weight gain, depression and a decrease in sexual desirability and satisfaction. These stories are not true.
A hysterectomy, by removing the cause of some painful, uncomfortable and weakening symptoms, gives most women a new lease of life; physically, mentally and sexually.
Contact numbers
If you need further advice or have any problems, please telephone either the Day Case Unit, where you had your operation, or the Surgical Decisions Unit:
University Hospital of North Tees
Day Case Unit
Telephone: 01642 624168
Monday – Thursday, 6.30am – 10.00pm
Friday, 6.30am – 9.00pm
Surgical Decisions Unit Reception
Direct Line: 01642 624566 / 01642 624628
24 hours, 7 days a week
University Hospital of Hartlepool
Day Case Unit
Telephone: 01429 522259
Mon-Thursday, 9.00am-9.00pm
Friday, 9.00am-5.00pm
Surgical Decisions Unit Reception
Direct Line: 01642 624566 / 01642 624628
24 hours, 7 days a week
If you have any worries or concerns, you should contact your GP during normal surgery hours. Outside surgery hours you should contact your GP’s surgery for the Out of Hours Service number.
Comments, concerns, compliments or complaints
Patient Experience Team (PET)
We are continually trying to improve the services we provide. We want to know what we’re doing well or if there’s anything which we can improve, that’s why the Patient Experience Team (PET) is here to help. Our Patient Experience Team is here to try to resolve your concerns as quickly as possible. The office is based on the ground floor at the University Hospital of North Tees if you wish to discuss concerns in person. If you would like to contact or request a copy of our PET leaflet, please contact:
Telephone: 01642 624719
Freephone: 0800 092 0084
Opening hours: Monday to Friday, 9:30am to 4:00pm
Email: [email protected]
Out of hours
Out of hours if you wish to speak to a senior member of Trust staff, please contact the hospital switchboard who will bleep the appropriate person.
Telephone: 01642 617617
Data protection and use of patient information
The Trust has developed Data Protection policies in accordance with Data Protection Legislation (UK General Data Protection Regulations and Data Protection Act 2018) and the Freedom of Information Act 2000. All of our staff respect these policies and confidentiality is adhered to at all times. If you require further information on how we process your information please see our Privacy Notices.
Telephone: 01642 383551
Email: [email protected]
Privacy NoticesLeaflet feedback
This leaflet has been produced in partnership with patients and carers. All patient leaflets are regularly reviewed, and any suggestions you have as to how it may be improved are extremely valuable. Please write to the Clinical Governance team, North Tees and Hartlepool NHS Foundation Trust, University Hospital of North Tees, TS19 8PE or:
Email: [email protected]
Leaflet reference: PIL1265
Date for review: 058/10/2023
