Information for patients
This leaflet can be made available in other formats including large print, CD and Braille and in languages other than English, upon request.
This leaflet tells you about an Endoscopy for your child.
What is an Endoscopy?
An endoscopy is the name of an examination where a thin flexible camera (an endoscope) is passed through your child’s mouth and down into their stomach.
For children this will be carried out under a general anaesthetic (a state of carefully controlled and supervised unconsciousness that means your child is unable to feel any pain).
How long will it take?
The examination itself will take approximately 10 to 20 minutes.
However, your child will be away from you for longer than this while they are waking up from the general anaesthetic.
What are the risks and possible complications?
The risks and possible complications include:
- Feeling bloated and sore throat. Your child may feel bloated and have a sore throat for 24 to 48 hours.
- Damage to teeth. The endoscope can occasionally cause damage to teeth. This is rare and a mouth-guard is used to reduce the risk.
- Bleeding. 1 patient in every 1,000 can suffer from bleeding. If any bleeding occurs during your child’s endoscopy steps will be taken to stop it. This may need a blood transfusion, or rarely, an operation.
- Perforation (hole). 1 patient in every 15,000 can suffer a perforation in the wall of the oesophagus, stomach or duodenum. If this happens your child may need an operation to repair it.
- Aspiration. If your child’s stomach contains food or drink it can leak into their lungs, affect their breathing and cause an infection.
How can I help to prepare my child?
Before your child’s examination you must:
- Tie back long hair for comfort.
- Remove any nail varnish.
- Remove any make-up.
- Remove all jewellery.
Please do not bring any valuables with your child.
What will happen when we arrive for my child’s
appointment?
An anaesthetist will discuss this with you and your child on the
morning of their examination.
You will have been given “magic” numbing cream which you should put on the back of your child’s hands before coming to hospital. This will help to reduce the pain your child may experience when a cannula is inserted.
When you arrive at the Paediatric Unit, you and your child will be introduced to nursing staff and a play specialist who will be looking after your child for the day.
A nurse will check your child’s personal details, ask questions about their health, check their blood pressure and pulse and explain the examination and risks to you. This is just to make sure you understand everything before you sign the consent form.
You should tell the nurse if your child has had any allergies or
reactions to drugs or other tests in the past and of any previous
endoscopies.
What will happen during my child’s examination?
If your child has a gas induction:
A clear mask will be placed over your child’s face and your child will breathe in the anaesthetic.
If your child has drug induction
Medication will be given directly into your child’s cannula (a fine tube inserted into a vein in the back of your child’s hand or arm using a small fine needle).
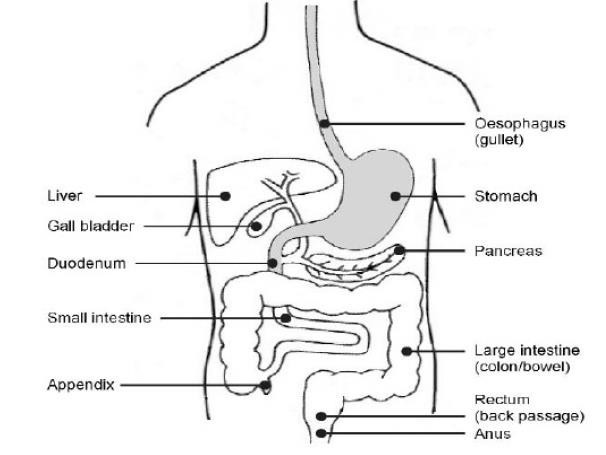
An endoscope (a thin, flexible tube) is passed into your child’s mouth and guided into their stomach. It allows the consultant to look at your child’s oesophagus (gullet), stomach and duodenum (small intestine) by passing back the pictures to a monitor.
This gives the consultant a clear view and enables them to see if there are any problems. Biopsies (small pieces of tissue) can be taken at the same time, if needed. Taking the biopsies will not hurt your child in any way.
We routinely take photographs or videos of your child’s insides during this procedure. These are used to help in your child’s investigations and treatment. The pictures taken during the examination will be kept as part of your child’s healthcare record.
Can I go to theatre with my child?
You and your child will go to theatre with a play specialist from the unit. Your child’s name band and details will be checked by theatre nurses, then you will go to the anaesthetic room where the anaesthetic will be given.
While your child is in theatre the play specialist will take you back to the unit to wait until your child returns.
What should my child wear?
Your child should wear comfortable, loose fitting bottoms such as leggings or jogging bottoms, but not a “onesie”. Your child may go to theatre in their own clothes but sometimes a theatre gown may be needed.
What will happen after the examination?
Your child will be taken to the recovery area where they will be able to rest until the effects of the general anaesthetic has worn off. A nurse will collect them and take them back to the unit.
Your child will be offered a drink and something to eat when they are ready.
Usually, if your child is not sick, their cannula is removed and you may take them home after about 1 hour.
When will I be told the result of my child’s
examination?
Before you leave the unit your child’s doctor will explain the results of their examination and any further plans. If your child had any biopsies taken and sent to a laboratory for further examination, you may have to wait for up to 6 weeks for the results.
If needed, you may be sent an outpatient appointment through the post to discuss the results of your child’s endoscopy in more detail.
A copy of your child’s results will also be sent to their GP.
How will my child feel when they get home?
Your child may feel tired due to the effect of the anaesthetic. Do not worry, they should relax quietly at home for the rest of the day. Your child can eat, drink and take any medication as usual after their examination.
Your child may have some abdominal discomfort due to the air put into their stomach during the examination. This usually settles within 24 hours.
If your child vomits, you may notice a small trace of blood for up to 72 hours afterwards. This can be a result of the biopsies taken and is normal.
You must contact the Paediatric Day Unit immediately (see
contact numbers) if your child:
- Has severe pain in their abdomen.
- Develops a temperature higher than 37.5ᵒC (99.5ᵒF).
If the department is closed and your child has an urgent problem the night after their procedure, you should contact your local Emergency Department.
Contact numbers
University Hospital of North Tees
Children and Young Person’s Emergency Department
Telephone: 01642 624533
24 hours a day, 7 days a week
If you have any worries or concerns you should contact your GP during normal surgery hours. Outside surgery hours, you should contact your GP’s surgery for the Out of Hours service number.
Comments, concerns, compliments or complaints
Patient Experience Team (PET)
We are continually trying to improve the services we provide. We want to know what we’re doing well or if there’s anything which we can improve, that’s why the Patient Experience Team (PET) is here to help. Our Patient Experience Team is here to try to resolve your concerns as quickly as possible. The office is based on the ground floor at the University Hospital of North Tees if you wish to discuss concerns in person. If you would like to contact or request a copy of our PET leaflet, please contact:
Telephone: 01642 624719
Freephone: 0800 092 0084
Opening hours: Monday to Friday, 9:30am to 4:00pm
Email: [email protected]
Out of hours
Out of hours if you wish to speak to a senior member of Trust staff, please contact the hospital switchboard who will bleep the appropriate person.
Telephone: 01642 617617
Data protection and use of patient information
The Trust has developed Data Protection policies in accordance with Data Protection Legislation (UK General Data Protection Regulations and Data Protection Act 2018) and the Freedom of Information Act 2000. All of our staff respect these policies and confidentiality is adhered to at all times. If you require further information on how we process your information please see our Privacy Notices.
Telephone: 01642 383551
Email: [email protected]
Privacy NoticesLeaflet feedback
This leaflet has been produced in partnership with patients and carers. All patient leaflets are regularly reviewed, and any suggestions you have as to how it may be improved are extremely valuable. Please write to the Clinical Governance team, North Tees and Hartlepool NHS Foundation Trust, University Hospital of North Tees, TS19 8PE or:
Email: [email protected]
Leaflet reference: PIL1144
Date for Review: March 2027
